

Mental Health
Mental health: why a ‘bad trip’ with ketamine treatment isn’t what you think it is.
Editor's Note
Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.
Please see a doctor before starting or stopping a medication.
If you have experienced emotional abuse, the following post could be potentially triggering. You can contact the Crisis Text Line by texting “START” to 741741.
It was Wednesday and time for my ketamine treatment . There is a certain amount of routine to getting my treatments. When I started with ketamine I thought I would get the IV treatments once every three months or so. That’s what everything I had read said would happen. Maybe the “treatment-resistant” part of my bipolar disorder applies to ketamine too. I don’t know. In any case, we have determined that every other week works for me. By the beginning of the second week, I start to dip in mood. I can reach suicidal thinking by the time it’s time for the next infusion. We try not to let me get to that place.
The infusions are accompanied by psychedelic “trips.” That’s just part of ketamine. In the beginning, I believed that the trip didn’t matter — the drug got in me regardless of if the trip was “good” or “bad.” A lot of my trips are “bad.” I believe this is largely because of complex post-traumatic stress disorder ( C-PTSD ). I put bad in quotes because it’s not an accurate description. The trips can be scary. I see things and feel things that are frightening or unpleasant. I have been literally terrified several times. That doesn’t mean they’re bad, though.
The trip before last Wednesday’s infusion was terrifying. I screamed so hard that I lost my voice for almost a full week. I just screamed and screamed. I was certain that I was permanently trapped in this other world that I was hallucinating. The people in the room with me, the nurses and anesthetist, looked like stick figures. They were walking around and they were talking. I didn’t know what they were saying; I was too busy screaming, “Please, somebody, notice that I’m still trapped over here in this alternate universe. Let me out!” One of them was telling me I was OK. I was insisting, “I am not OK.” As the ketamine wore off, I returned to this world and realized everything was fine. Just like every other time.
When it was time for the next infusion two weeks later, the clinic director decided to have a nurse, Colleen, sit with me for the trip. The thinking was I would feel safer and stay calmer. Maybe not scream my head off. Colleen is special to me; she has been with me since my first infusion. She has held my hand many times when trips turned frightening, always reminding me “you are safe.” It was a logical and welcome decision to have Colleen sit with me.
Except in this trip, Colleen turned evil. The world was red and black, no other colors. The walls in the room looked like the walls in “The Matrix” with green code running down black walls. Except my “code” was red. Colleen was red and terrifying. She was saying terrible things. I was convinced that the clinic was a front for an evil organization trying to do mind control and keep me trapped in that cold, black-and-red world forever. I didn’t scream because Colleen was there. I was afraid of her. I was afraid of what might happen if I screamed. What would she do to me?
Coming out of that trip, I was convinced that it would be my last. I couldn’t keep doing this, I didn’t trust anyone; that’s part of C-PTSD after all. I sent the clinic director an email the next day and asked him if he could sedate me for my next trip. Sometimes when I get especially agitated during a trip, he will add in a little sedative toward the end. When he does that, I go home with little to no memory of anything that happened during the trip. He wisely answered that the trips were important; he wanted me to experience them.
And he’s right because here’s the thing. Those “bad” trips? They aren’t bad. They’re unpleasant. They’re scary. They’re challenging and very hard to go through. But they aren’t bad. Let me explain.
The day after the Red Colleen (sorry, Colleen) trip, I went to dinner with a friend. We talked about a lot of things. This was the first time we had gotten together since my suicide attempt two months earlier. I filled her in on what it was like when I made the attempt, the ambulance ride, the emergency room, the week spent on the medical floor of the hospital, and the week after that on the psychiatric floor. I walked her through all of it. On my drive home after dinner, I had to pull into a parking lot because I was so overcome with emotion that I couldn’t keep driving. I sat in the parking lot and sobbed, letting out all the emotion that had come up while talking to my friend. It was a good, cleansing cry. When I was composed enough to drive, I made my way home. Turned out, that cry was just the beginning.
Later that same night, after everyone had gone to bed, I was up by myself. I put YouTube on the television and played my favorite music video. I had discovered this video months earlier and it had become a constant as a self-care thing I did. This video could make me cry, it could make me laugh. Something about the music touched me deep in my soul; I physically felt the music. As it played this night, tears started to flow. And I let them.
That’s something my therapist has been working on with me for over a year: Feel the feelings. Don’t avoid them, don’t push them away. Stop the struggle. Feel them. As the song came to its end, I started to smile through my tears. This is an amazing piece of music. The next video started to play. I cried some more. For the next half hour, I cried as I listened to and felt the music. But I didn’t just cry. I was turned inside out. Something broke inside me. I sobbed. I laughed. I cried about the suicide attempt. I cried about the time in the hospital. I cried about how hard the past two years have been as I rapid-cycled through bipolar , up and down, going through six different medications on the way to being declared treatment-resistant and getting off all drugs. How much work I had done with my therapist, working through all the trauma of my childhood. And I kept crying.
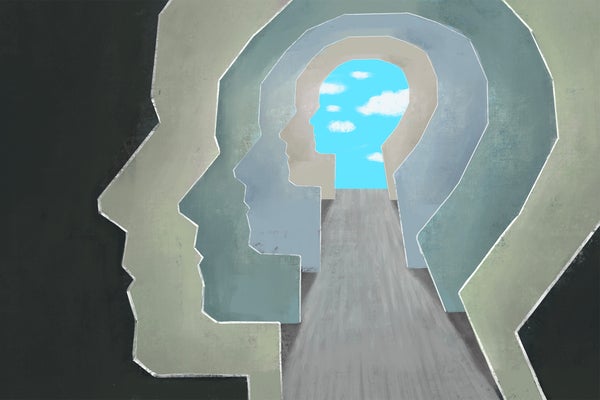
Then I remembered my therapist had suggested the day before that I do a meditation we know called “Working with Difficulty.” It walks you through grounding like normal. But then the guide suggests that you take any negative emotion that is coming up and place it on the worktable of your mind. Find the physical sensations of it in your body. Where are you feeling this emotion?
The guide instructs that you don’t do anything to change your breathing, just notice it, focus on it. I was sobbing hysterically. And I kept sobbing. I was breathing; it was just sobs and hyperventilating, not the calm, controlled breathing I think of when I think of meditating. I let myself do it. I gave myself permission to feel this. To express it. As I worked through this 25-minute meditation, I let myself feel all of it. And as the crying continued, that traumatized little girl who had never been allowed to cry showed up. She started to cry. This is the miracle of ketamine: It allows your mind to do things it hasn’t been able to do before. That little girl had been shamed into never crying . It wasn’t allowed. And she desperately needed to cry. She was not going to be able to heal from the trauma until she could express all that she had stuffed so far down for so long. And I was able to give her permission. I encouraged her: yes, dear one, cry. Cry until you don’t have any tears left to cry.
And she did. She cried. She rocked back and forth. She hugged a pillow and sobbed into it. I don’t have words to describe what this experience was like. The intensity was beyond description. There was one point when I felt I was back in the psychedelic part of the ketamine trip. It’s like ketamine lets your mind open in places it hasn’t opened before. This gave me the space and the permission I needed to let this little girl cry her heart out.
This was such a healing episode. I’m not the same today. I’ve been used to learning coping skills in therapy. I assumed that was the best I could hope for — learning how to cope. But, no. This was healing. The pain that that little girl had held inside all these years was released. This isn’t the first time I’ve had such a physical reaction and release of repressed pain. And it is ketamine that allowed this — caused it.
As I said in the beginning, I believe there’s no such thing as a bad trip. Every trip I’ve had that was painful ended with something good. A new insight. An expression of long-buried pain. I feel it necessary to say that I have not arrived at these good results alone. I have needed the guidance of the people at the clinic. I have needed my therapist. I have needed my psychiatrist. I don’t know psychedelics. Had I done these trips on my own, I think I would have ended up further traumatized. These trips can get very difficult and very intense. But my subconscious has been hard at work during them. Things have bubbled to the surface — the conditioned emotional responses, the fight-or-flight triggers, the repressed memories, they have been in my mind all along. Ketamine, along with therapy, has allowed those things to surface and be dealt with. It’s a very powerful and healing combination.
For more on ketamine treatments for depression, bipolar disorder, trauma and other mental illnesses, see The Mighty Community’s posts here .
If you or a loved one is affected by domestic violence or emotional abuse and need help, call The National Domestic Violence Hotline at 1-800-799-7233
We want to hear your story.
Do you want to share your story? Click here to find out how.
Photo by Just Jack on Unsplash
Early childhood trauma and lifelong struggles with mental health led me to The Mighty. I've learned the power of sharing and not staying in this madness alone. Sometimes I can support, sometimes I need support.
Ketamine trips are uncannily like near-death experiences
Photo by JR Korpa/Unsplash
by Christian Jarrett + BIO
First-hand accounts of what it is like to come close to death often contain the same recurring themes, such as the sense of leaving the body, a review of one’s life, tunnelled vision and a magical sense of reality. Mystics, optimists and people of religious faith interpret this as evidence of an afterlife. Skeptically minded neuroscientists and psychologists think that there might be a more terrestrial, neurochemical explanation – that the profound and magical near-death experience (NDE) is caused by the natural release of brain chemicals at or near the end of life.
Supporting this, observers have noted the striking similarities between first-hand accounts of NDEs and the psychedelic experiences described by people who have taken mind-altering drugs.
Perhaps, near death, the brain naturally releases the same psychoactive substances as used by drug-takers, or substances that act on the same brain receptors as the drugs. It’s also notable that psychedelic drugs have been taken by the shamans of traditional far-flung cultures through history as a way to, as they see it, visit the afterworld or speak to the dead.
To date, however, much of the evidence comparing NDEs and psychedelic trips has been anecdotal or based on questionnaire measures that arguably struggle to capture the complexity of these life-changing experiences. Pursuing this line of enquiry with a new approach, an international team of researchers led by Charlotte Martial at the University Hospital of Liège in Belgium has conducted a deep lexical analysis , comparing 625 written narrative accounts of NDEs with more than 15,000 written narrative accounts of experiences taking psychoactive drugs ( sourced from the Erowid Experience Vaults, a US-based non-profit that documents psychoactives), including 165 different substances in 10 drug classes.
The analysis, published online in Consciousness and Cognition in February 2019, uncovered remarkable similarities between the psychological effects of certain drugs – most of all ketamine, but also notably the serotonergic psychedelic drugs such as LSD – and NDEs. Indeed, the five most common category terms in the narrative accounts of people who’d taken ketamine were the same as the five most common in the accounts of NDEs, suggesting ‘shared phenomenological features associated with an altered state of perception of the self and the environment, and a departure from the everyday contents of conscious mentation’.
From category to category, the semantic similarity is profound. When referring to perceptions, both groups used the words ‘face’ and ‘vision’. The emotional word most commonly used by both was ‘fear’. In the category of consciousness and cognition, drug-takers and participants who’d been close to death most often referred to words such as ‘reality’, ‘moment’, ‘universe’, and ‘learn’. The setting was often described as ‘door’ and ‘floor’. A negative tone emphasising unpleasant bodily sensations was a shared common theme, as well.
T he findings back up the observations of some of the most famous 20th-century explorers of the psychedelic world – the American psychologist Timothy Leary described trips as ‘experiments in voluntary death’, and the British-born writer and philosopher Gerald Heard said of the psychedelic experience: ‘That’s what death is going to be like. And, oh, what fun it will be!’ But claims about the similarities go beyond these famous reports. The new research legitimises the long-standing analogy between the experience of dying and the acute effects of certain psychoactive drugs. Links between dying, death, a potential existence of afterlife and certain hallucinogenic plants and fungi emerged independently across different societies, and are also ubiquitous in contemporary psychedelic culture. However, empirical research has been scarce, until now.
To an extent, the results also support neurochemical accounts of NDEs, and especially the controversial proposal that such experiences are caused by the natural release of an as-yet-to-be-discovered ketamine-like drug in the brain (adding plausibility to this account, ketamine is known to act on neural receptors that, when activated, help to prevent cell death and offer protection from lack of oxygen).
‘This body of empirical evidence supports that near-death is by itself an altered state of consciousness that can be investigated using quantitative psychometric scales,’ the researchers say. That in itself is quite a realisation. As they note wryly, ‘Unlike other human experiences, dying is difficult to study under controlled laboratory conditions by means of repeated measurements,’ making it a challenge to investigate NDEs experimentally. Although the new research lacks laboratory control, on the plus side, the lexical comparison that Martial’s team conducted is ‘massive both in terms of the investigated drugs and the number of associated reports’.
The limitations of the current approach, including a reliance on retrospective reports, often decades-old, means, as the researchers put it, that they cannot validate nor refute the neurochemical models of NDEs. ‘However,’ they add, ‘our results do provide evidence that ketamine, as well as other psychoactive substances, result in a state phenomenologically similar to that of “dying” (understood as the content of NDE narratives). This could have important implications for the pharmacological induction of NDE-like states for scientific purposes, as well as for therapeutic uses in the terminally ill as means to alleviate death anxiety. We believe that the development of evidence-based treatments for such anxiety is a cornerstone of a more compassionate approach towards the universal experience of transitioning between life and death.’
They also warn experimenters to be prepared and beware. ‘The intensity of the experience elicited by [ketamine] relative to cannabis may represent a shock to unsuspecting users, who could retrospectively report the belief of being close to death,’ the researchers say. Pot-smokers, you’ve been warned. As one of the most intense and life-changing altered states known, an NDE is no toke on a pipe after class or work.
This is an adaptation of an article originally published by The British Psychological Society’s Research Digest.

Gentle medicine could radically transform medical practice
Jacob Stegenga

Childhood and adolescence
For a child, being carefree is intrinsic to a well-lived life
Luara Ferracioli

Meaning and the good life
Sooner or later we all face death. Will a sense of meaning help us?
Warren Ward

Philosophy of mind
Think of mental disorders as the mind’s ‘sticky tendencies’
Kristopher Nielsen

Philosophy cannot resolve the question ‘How should we live?’
David Ellis
Love and friendship
Your love story is a narrative that gets written in tandem
Pilar Lopez-Cantero
July 3, 2024
Is a Drug Even Needed to Induce a Psychedelic Experience?
A Stanford anesthesiologist deconstructs the component parts of what it means to undergo a psychedelic trip
By Gary Stix
Jorm Sangsorn/Getty Images
A debate has long percolated among researchers as to whether what happens after taking a psychedelic drug results from the placebo effect—rooted in a person’s belief that taking psilocybin or ketamine is going to give them a transformative experience. Boris D. Heifets, an associate professor of anesthesiology at the Stanford University School of Medicine, has been tackling this question amid his broader laboratory investigations of what exactly happens in mind and brain when someone takes a psychedelic . How much of this sometimes life-altering experience is chemical and empirical, and how much is mental and subjective? It turns out the effects may consist of a lot more than just a simple biochemical response to a drug activating, say, the brain’s serotonin receptors. Heifets recently talked with Scientific American about his years-long quest to define the essence of the psychedelic experience.
[ An edited transcript of the interview follows .]
Are we coming any closer to understanding how psychedelics work and how they work in the context of therapy. Are we closer to using these transformational experiences to treat psychiatric disorders?
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Having been in this field for a while, there’s still this inescapable problem of how to study psychedelics. One framework that I find very useful is thinking about it in three categories.
There's the biochemical drug effect, which interacts with basic brain biology—chemicals interacting with receptors on cells. That happens whether or not you can “feel” the effect of the drug. Then there is the conscious experience related to changes in sensation and revelatory, hallucinatory and ecstatic feelings. These experiences are closely tied to taking the drug, and usually we think of them as caused by the drug. But it is actually quite difficult to say whether a lasting change in mood or outlook was a result of the drug—a biochemical effect—or the trip itself, the experiential effect.
The third factor, then, is all of those aspects of the overall drug experience that are independent of the drug or trip—the non-drug factors, what [psychologist and psychedelics advocate] Timothy Leary called the “set and setting.” How much does your state of mind and the setting in which you take a drug influence the outcome? This category includes expectations about improvement in, say, your depression, expectations about the experience, the stress level in the environment. It would also include integration, making sense of these intense experiences afterward and integrating them into your life. And it’s useful to put each of these things in its own box because I think each of them is somewhat isolated. The goal is to make each box smaller and smaller, to really deconstruct the pieces.
So how have you gone about examining all this?
One example of how we’ve used this framework in our research is an experiment in which we gave [participants with depression] ketamine during general anesthesia . The idea was to explore just the biochemical drug effect by blanking out conscious experience to see whether people got better from their depression.
Our intention with this experiment was to get at this question that a lot of people have been asking: Is it the drug or the trip that is making someone better? You can address that question in a couple of different ways. One is to redesign the drug to eliminate the trip. But that is a very long process. As an anesthesiologist, my solution of course was to address the problem with the use of general anesthesia. We used the anesthetics to basically suppress conscious experience of the associated psychological effects of ketamine, which many people think may be relevant and even crucial to the antidepressant effects.
We collaborated closely with psychiatrists Laura Hack and Alan Schatzberg, [both] at Stanford, and we designed this study to look like every ketamine study in the past 15 years. We picked the same type of participants: [people] with moderate to severe major depressive disorder who had failed other treatments for moderate or severe depression. We administered the same questionnaires; we gave the same dose of ketamine.
The difference was these participants happened to be coming in for surgery for hips, knees, hernias, and while they were under general anesthesia, we gave them a standard antidepressant dose of ketamine. Because the patients were under anesthesia and couldn’t tell whether they were on a drug or not, this may have been the first blinded study of ketamine.
What was surprising was that the placebo group [who received no ketamine] also got better, indistinguishably from those who received the drug. Almost 60 percent of the patients had their symptom load cut in half, and there was at least 30 percent remission from major depressive disorder. These were patients who had been sick for years, and that finding was a big surprise. In a sense, it was a failed trial in that we couldn't tell the difference between our two groups.
What I take from that is really that this doesn't say much about how ketamine works. What it does say is just how big a therapeutic effect you can attribute to nondrug factors. That’s what people call the placebo effect.
It’s a word that describes everything from sugar pills to our surgeries. In our case, it may have had something to do with the preparation for the surgery. We messaged patients early; we engaged with them early. They weren’t used to people being interested in their mental health.
What did you discuss?
We talked to them for hours; we heard about their histories; we got to know them. I think they felt seen and heard in a way that many patients don’t, going into surgery. I’m thinking about parallels with the preparation steps for psychedelic trials. Patients in both types of research are motivated to be in these studies. In our study, they were told that they were testing the therapeutic potential of a drug and that there was a 50–50 chance they might get it. And then there was the big event of actually having the surgery. In this case, it was similar to having a psychedelic trial—a big, stressful, life-impacting event.
The patients closed their eyes and opened them after the surgery, and in many cases, they had the sense that no time had passed. They knew they went through something because they had the bandages and scars to prove it. What I take from that is that these nondrug effects, such as expectations of a particular outcome, are almost certainly present in most psychedelic trials and are independently able to drive a big therapeutic effect.
It became obvious that people had powerful experiences. Most people don't spontaneously improve from years of depression. After surgery, they get worse. That's what the data show. And the fact that we're able to make this degree of a positive impact after hours and hours of interpersonal contact and messaging, that’s important. This was a really clear demonstration to me that nondrug factors, such as expectations and feelings of hope, contribute a substantial portion to the effects we’ve seen. And you would be foolish to disregard those components in designing a therapy. And, you know, the truth is that most clinicians make use of these techniques every day in building a rapport with patients, leveraging this placebo response.
Does that suggest in any way that the effects of psychedelics might be substantially—or perhaps entirely—placebo effects?
So this is where I think you have to ask the question: What do we mean by placebo? Characteristically, people use the word placebo in a kind of a dismissive way, right? If a person responds to placebo, the subtle implication is there was nothing wrong. And that’s not what we’re talking about here.
Think about everyday situations that bring about life changes. A heart attack or near-death experience may cause someone in a high stress job to change their job and lifestyle habits—exercising and eating better. That all can be grouped under the label of a placebo effect.
Another possibility to achieve the same goal is having a transformational experience that you then use to make changes in your life. So the question is: How do you do this in a practical way? You can’t exactly go out and give people heart attacks or even send them on life-changing experiences, such as skydiving or on trips to the Riviera. But you can give them a psychedelic. That’s a big, powerful experience. In many cases, that is unique in some people’s lives and confers the opportunity to make changes for the better.
How does giving an actual psychedelic drug to someone in a clinical trial relate to the three categories you mentioned earlier?
Let’s circle back to this idea that psychedelic transformation could rely either on the biochemical effect, the experience of the trip itself, or nondrug factors. Our study of ketamine during anesthesia really highlighted the role of nondrug factors such as expectation but didn’t really get at the question of “Is it the drug or the trip?”
To answer that, some [of my] scientist colleagues are testing nonpsychedelics, or nonhallucinogenic psychedelic derivatives, to see whether patients with depression, for example, get better after treatment with a drug that can cause some of the same biochemical changes as a classical psychedelic but doesn’t have a “trip” associated with it. That’s “taking the trip out of the drug.” But what if you could “take the drug out of the trip,” meaning [the creation of] an experience that is reproducible across people that checks many of the same boxes as a classic psychedelic-induced trip but that doesn’t actually require the use of a psychedelic molecule? So what, in this context, you provide people with is a profound experience that can even be somewhat standardized so you can study it. And it would be powerful and vivid and meaningful and revelatory. Do you get the same types of effects?
That would not be definitive evidence. But it would strongly suggest that maybe there’s nothing intrinsically special about the activity of a drug that activates a particular receptor that mediates the effects of psychedelics. What that would do is put front and center the role of human experience in psychological transformation.
So you might be able to bypass the need for a psychedelic drug if you can get the same result with a nonpsychoactive drug?
Maybe you can—we just don’t know. That’s an empirical question.
To try to answer that question, I’ve worked closely with Harrison Chow, also an anesthesiologist at Stanford, on a protocol that we call “dreaming during anesthesia.” It's really a state of consciousness that happens before emergence from anesthesia. When patients awaken from surgery, they progress from a state that is deeper than sleep. And they pass through a number of conscious states, some of which produce dreams . They wake up, and about 20 percent of patients will have some dream memory imagery.
What we do is prolong that process and use EEG [electroencephalography] to home in on a specific biomarker of that state. We can hold someone in this preemergent state for 15 minutes. Participants wake up, and the stories they tell are very hard to ignore. These are some of the most vivid dreams they’ve ever had. They say things like “that was more real than real.” The participants with trauma dream of reintegrating their body map, reimagining their body [as] once again whole. We had a participant who had been assigned male at birth and had gender-affirming] surgery. She had been in the military and reimagined her life before her gender-affirming care. She saw herself doing high-intensity military training exercises, now with her body aligning with her gender.
These are intense experiences—vivid, emotionally salient, possibly hallucinatory. We published a couple of case reports now where we actually have seen therapeutic effects on a par with what we see in psychedelic medicine: powerful experiences followed by a resolution of symptoms in a psychiatric disorder.
What we’re seeing is a shared physiology in terms of EEG results for these dream states and the EEGs present for psychedelics. We see at least some shared phenomenology in terms of description of the experiences, and there are also similar therapeutic effects.
What are some of your next steps?
In addition to possibly producing a very compelling therapeutic using the common anesthetic propofol, we are working hard to develop experimental tools using anesthesia, using our knowledge of how placebo works in the brain to separate these three factors: the drug effect, the experiential effect and nondrug factors. At least two of those big effects, neither of which depends on administering a psychedelic, appear to be capable of generating a profound therapeutic impact that certainly would be sufficient on its own to claim the outcomes seen in psychedelic trials. And that, to me, shows that maybe the emphasis is misplaced when we're focused on reengineering the drug to get rid of hallucinogenic effects. We should be focused on reengineering the experience.
But we're still working on number three, the drug effect. We have collaborations with David Olson, a chemist at the University of California, Davis, who has pioneered the use of nonhallucinogenic psychedelics. We are helping to characterize the profound neuroplastic effects of a drug he has developed that appears, at least in mice, not to trigger the same type of brain activation that classical psychedelics do. What I’m trying to convey is that, using these approaches, we are able to get some traction to experimentally define, isolate and identify the components of this very complex therapeutic package we call psychedelic therapy.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
The ketamine economy: New mental health clinics are a 'Wild West' with few rules

Patients report that ketamine infusions can be lifesaving, with immediate improvement for severe depression. But dosage and safety measures vary widely at the hundreds of clinics that have opened. Yana Iskayeva/Getty Images hide caption
Patients report that ketamine infusions can be lifesaving, with immediate improvement for severe depression. But dosage and safety measures vary widely at the hundreds of clinics that have opened.
In late 2022, Sarah Gutilla's treatment-resistant depression had grown so severe that she was actively contemplating suicide. Raised in foster care, the 34-year-old's childhood was marked by physical violence, sexual abuse and drug use, leaving her with life-threatening mental scars.
Out of desperation, her husband scraped together $600 for the first of six rounds of intravenous ketamine therapy at Ketamine Clinics Los Angeles, which administers the generic anesthetic for off-label uses such as treating depression. When Gutilla got into an Uber for the 75-mile ride to Los Angeles, it was the first time she had left her home in Llano, Calif., in two years. The results, she says, were instant.
"The amount of relief I felt after the first treatment was what I think 'normal' is supposed to feel like," she says. "I've never felt so OK and so at peace."
For-profit ketamine clinics have proliferated over the past few years, offering infusions for a wide array of mental health issues, including obsessive-compulsive disorder, depression and anxiety. Although the off-label use of ketamine hydrochloride, a Schedule III drug approved by the Food and Drug Administration as an anesthetic in 1970, was considered radical just a decade ago, now between 500 and 750 ketamine clinics have cropped up across the United States.
Market analysis firm Grand View Research pegged industry revenues at $3.1 billion in 2022, and it projects them to more than double to $6.9 billion by 2030. Most insurance doesn't cover ketamine for mental health, so patients must pay out-of-pocket.
Off-label use
While it's legal for doctors to prescribe ketamine, the FDA hasn't approved it for mental health treatment, which means that individual practitioners develop their own treatment protocols. The result is wide variability among providers, with some favoring gradual, low-dosage treatments while others advocate larger amounts that can induce hallucinations, as the drug is a psychedelic at the right doses.
"Ketamine is the Wild West," says Dustin Robinson, the managing principal of Iter Investments, a venture capital firm specializing in hallucinogenic drug treatments.
Ketamine practitioners stress that the drug's emergence as a mental health treatment is driven by a desperate need. Depression is the leading cause of disability in the U.S. for individuals ages 15 to 44, according to the National Institute of Mental Health, and around 25% of adults experience a diagnosable mental disorder in any given year.

Shots - Health News
From chaos to calm: a life changed by ketamine.
Meanwhile, many insurance plans cover mental health services at lower rates than physical health care, despite laws requiring parity . Thus, many patients with mental health disorders receive little or no care early on and are desperate by the time they visit a ketamine clinic, says Dr. Steven Siegel , chair of psychiatry and the behavioral sciences at the University of Southern California's Keck School of Medicine.
Matthew Perry and Elon Musk
But the revelation that Friends star Matthew Perry died in part from a large dose of ketamine , as well as billionaire Elon Musk's open use of the drug , has piqued fresh scrutiny of ketamine and its regulatory environment, or lack thereof.
Commercial ketamine clinics often offer same-day appointments in which patients can pay out-of-pocket for a drug that renders immediate results. The ketamine is administered intravenously, and patients are often given blankets, headphones and an eye mask to heighten the dissociative feeling of not being in one's body. A typical dose of ketamine to treat depression, which is one-tenth the dosage used in anesthesia, costs clinics about $1, but clinics charge $600 to $1,000 per treatment.
Ketamine is still shadowed by its reputation as the party drug known as "Special K"; Siegel's first grant from the National Institutes of Health was to study ketamine as a drug of abuse. It has the potential to send users down a "K-hole," otherwise known as a bad trip, and can induce psychosis. Research in animals and recreational users has shown that chronic use of the drug impairs both short- and long-term cognition.
Perry's drowning death in October raised alarms when the initial toxicology screening attributed his death to the acute effects of ketamine. A December report revealed Perry received infusion therapy a week before his death but that the fatal blow was a high dose of the substance taken with an opioid and a sedative on the day of his death — indicating that medical ketamine was not to blame.
A variety of protocols
Sam Mandel co-founded Ketamine Clinics Los Angeles in 2014 with his father, Steven Mandel, an anesthesiologist with a background in clinical psychology, and Sam Mandel says the clinic has established its own protocol. That includes monitoring a patient's vital signs during treatment and keeping psychiatrists and other mental health practitioners on standby to ensure safety. Initial treatment starts with a low dose and increases if that is not effective.
While many clinics follow the Mandels' graduated approach, the dosing protocol at MY Self Wellness, a ketamine clinic in Bonita Springs, Fla., is geared toward triggering a psychedelic episode.
Christina Thomas, president of MY Self Wellness, says she developed her clinic's procedures against a list of "what not to do" based on the bad experiences that people have reported at other clinics.

A sign for a ketamine clinic that has four locations in South Florida. Between 500 and 750 similar clinics exist across the U.S., according to market research firm Grand View Research. Ricardo Ramirez Buxeda/Orlando Sentinel/Tribune News Service via Getty Images hide caption
A sign for a ketamine clinic that has four locations in South Florida. Between 500 and 750 similar clinics exist across the U.S., according to market research firm Grand View Research.
The field isn't entirely unregulated: State medical and nursing boards oversee physicians and nurses, while the FDA and Drug Enforcement Administration regulate ketamine. But most anesthesiologists don't have a background in mental health, while psychiatrists don't know much about anesthesia, Sam Mandel notes. He said a collaborative, multidisciplinary approach is needed to develop standards across the field, particularly because ketamine can affect vital signs such as blood pressure and respiration.
The protocols governing Spravato, an FDA-approved medication based on a close chemical cousin of ketamine called esketamine, are illustrative. Because it has the potential for serious side effects, it falls under the FDA's Risk Evaluation and Mitigation Strategies (REMS) program, which puts extra requirements in place, says Iter Investments' Robinson. Spravato's REMS requires two hours of monitoring after each dose and prohibits patients from driving on treatment days.

Nasal Spray Is A New Antidepressant Option For People At High Risk of Suicide
Generic ketamine, by contrast, has no REMS requirements. And because it is generic, cheap and already on the market, drugmakers have little financial incentive to undertake the costly clinical trials that would be required for FDA approval for specific psychiatric conditions.
That leaves it to the patient to assess ketamine providers. Clinics dedicated to intravenous infusions, rather than offering the treatment as an add-on, may be more familiar with the nuances of administering the drug. Ideally, practitioners should have mental health and anesthesia expertise or have multiple specialties under one roof, and clinics should be equipped with hospital-grade monitoring equipment, Mandel says.
The University of Southern California's Siegel, who has researched ketamine since 2003, said the drug is especially useful as an emergency intervention, abating suicidal thoughts for long enough to give traditional treatments, like talk therapy and SSRI antidepressants, time to take effect.
"The solutions that we have and have had up until now have failed us," Mandel says.
The drug is now popular enough as a mental health treatment that the name of Mandel's clinic is a daily sight for thousands of Angelenos, as it appears on 26 Adopt A Highway signs along the 405 and 10 freeways.
And the psychedelic renaissance in mental health is accelerating. A drug containing MDMA, known as ecstasy or molly, is expected to receive FDA approval in 2024. A drug with psilocybin, the active ingredient in "magic mushrooms," could launch as early as 2027, the same year a stroke medicine with the active ingredient DMT, a hallucinogen, is expected to debut.

Psychedelic drugs may launch a new era in psychiatric treatment, brain scientists say
Iter Investments' Robinson says many ketamine clinics have opened in anticipation of the expanded psychedelic market. Since these new drugs will likely be covered by insurance, Robinson advises clinics to offer FDA-approved treatments such as Spravato so they'll have the proper insurance infrastructure and staff in place.
For now, Sarah Gutilla will pay out-of-pocket for ketamine treatments. One year after her first round of infusions, she and her husband are saving for her second. In the meantime, she spends her days on her ranch in Llano, where she rescues dogs and horses and relies on telehealth therapy and psychiatric medications.
While the infusions aren't "a magic fix," they are a tool to help her move in the right direction.
"There used to be no light at the end of the tunnel," she says. "Ketamine literally saved my life."
This article was produced by KFF Health News , a national newsroom that produces in-depth journalism about health issues. KFF Health News is the publisher of California Healthline , an editorially independent service of the California Health Care Foundation .
- mental health
- Obsessive Compulsive Disorder
- psychedelic drugs
What Is Ketamine and Is It Effective for Depression?
Find out what ketamine is, how ketamine therapy is used to treat depression, what side effects it can have and more.
This article is based on reporting that features expert sources.
What Is Ketamine?
After the death of actor Matthew Perry, ketamine, a longtime party drug, came into the public eye for a new reason. Perry had been undergoing ketamine infusion therapy for depression, which has been determined as a contributing factor in his death. Ketamine, initially recognized for its potent anesthetic and dissociative properties, has emerged as a treatment for depression .

Getty Images
Perry's death has raised questions about the increasing reliance on ketamine by doctors who see it as a promising alternative therapy for depression and other mental health disorders , although its long-term benefits and effects have not been well researched.
To the everyday person, a depression diagnosis might seem straightforward: symptoms of a persistent sad mood , lack of energy and little enjoyment in pleasurable activities, all to be remedied by psychotherapy and a medication. However, it's not so simple.
Dr. Ryan Sultan, a teaching psychiatrist, research scientist and the director of mental health informatics at Columbia University Irving Medical Center/New York State Psychiatric Institute in New York, explains that depression is a complex condition with various subtypes, impacted by genetics and other underlying factors.
Given the complexity of the diagnosis, any additional tool – such as ketamine – in the therapeutic arsenal is helpful. It might end up as the most successful treatment for an individual, finally alleviating their depressive symptoms.
Ketamine is a powerful medication that has been safely used in medical and veterinary science for over a century, mainly as an anesthetic. Ketamine can induce a state of sedation (feeling calm and relaxed), immobility, relief from pain, hallucinations and amnesia. It has gained recent popularity for treating depression. Ketamine is short for ketamine hydrochloride, which the Drug Enforcement Administration considers a Schedule III controlled substance, meaning it has the potential for abuse and dependence.
There are various formulations of ketamine. Ketamine is a mixture of two molecules called R-ketamine and S-ketamine, sometimes referred to as arketamine and esketamine, respectively. All formulations of ketamine, except Food and Drug Administration-approved Spravato, are being used off-label when used for the treatment of depression.
The Food and Drug Administration circulated a press release on October 10, 2023, stating, "Ketamine is not FDA approved for the treatment of any psychiatric disorder. FDA is aware that compounded ketamine products have been marketed for a wide variety of psychiatric disorders (e.g., depression, anxiety, post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder); however, FDA has not determined that ketamine is safe and effective for such uses."
Currently, ketamine is considered on-label only for anesthesia.
The FDA has not approved ketamine for depression, except for the nasal spray form of ketamine called Spravato, which it approved in 2019. There are currently no confirmed plans to approve other forms of ketamine for the treatment of depression, but as more research continues, this may change. Spravato is "approved as a nasal spray for treatment-resistant depression in adults and for depressive symptoms in adults with major depressive disorder with acute suicidal ideation or behavior (in conjunction with an oral antidepressant)," according to the FDA's press release.
What Types of Depression Is Ketamine Therapy Used for?
Ketamine is primarily used for a type of depression called treatment-resistant depression . TRD is a type of major depressive disorder that doesn't respond to traditional first-line treatment, like selective serotonin reuptake inhibitors, such as Prozac or Zoloft.
Ketamine therapy can be effective for some patients, says Dr. Helen Lavretsky, professor of psychiatry in-residence at the David Geffen School of Medicine at UCLA. She's also director of the Late-Life Mood, Stress and Wellness Research Program and director of the Integrative Psychiatry Clinic.
"Ketamine use should be reserved for truly treatment-resistant patients who failed to respond to two or more antidepressants administered in the optimal dose for at least two to four months," she says.
How Does Ketamine Therapy Help With Depression Symptoms?
Dr. Martha Koo, the founder and chief medical officer at Neuro Wellness Spa and a board-certified provider in psychiatry and addiction medicine based in Manhattan Beach, California, says that the reputation of ketamine being a party drug and a horse tranquilizer may cause some skepticism.
Ketamine is in a drug class called dissociative anesthetics, and ketamine is specifically an N-methyl-D-aspartate receptor antagonist. Koo explains that this means that ketamine acts on the glutamatergic system in the brain, which is responsible for:
- Growing new pathways and connections between brain cells, called neuronal growth
- Maintaining neuroplasticity, which is the ability to learn new skills and become better at them
- Helping different parts of the brain work together as a team, called neuronal interconnectivity
- Helping you feel energized and focused, while also maintaining a sense of calm
With ketamine giving a boost to the glutamatergic system, it may help people struggling with depression to feel like their brain is working more harmoniously, giving them energy, strength and focus to be able to face the day.
Is Ketamine Effective for Depression?
Ketamine administered intravenously – which can involve up to six infusions – has shown positive effects in patients within a few hours, relieving depressive symptoms and suicidal thoughts, says Lavretsky. Intravenously administered ketamine can quickly resolve "depressive symptoms and suicidal ideations" in patients under 65 years old, she says. "However, the need for IV access and physician monitoring limits its uses. In addition, the medication's long-term use efficacy and safety are not well known."
In addition, "it's important to acknowledge that as ketamine treatments have been administered to broader populations, there has been variability in its effectiveness," notes Sultan.
Research suggests that ketamine administered through the nose (Spravato) or taken orally requires two to four weeks of treatment before taking effect.
The effects of ketamine depend on the individual, the type of ketamine they received and the dosage. The body will eliminate ketamine in a matter of hours, but the effects of it may last for more time, up to a week or longer.
Ketamine dosage and frequency
There are a few routes and types of medications for ketamine for depression. In the October 2023 press release, the FDA reiterates, "Compounded drugs, including compounded ketamine products, are not FDA approved, which means FDA has not evaluated their safety, effectiveness or quality prior to marketing. Therefore, compounded drugs do not have any FDA-approved indications or routes of administration."
This means there are no FDA-regulated routes or dosages for ketamine, except in the case of FDA-approved Spravato. But, here are some of the typical routes of administration and dosages that health care providers may use:
- Intravenous ketamine. Koo says that IV ketamine works the fastest, with symptom relief within a few hours. IV ketamine doses are weight-dependent and commonly administered at 0.5 mg/kg. Dr. Danielle Greenman, a functional medicine physician and head of ketamine-assisted psychotherapy at Blum Center for Health in New York, says IV ketamine peaks around one minute, and many providers prefer IV ketamine due to its rapid onset, ability for more precise dosing and fewer side effects.
- Intramuscular ketamine. Ketamine can also be given as a shot into the muscle, usually in the upper outer gluteus. A standard IM dose is 0.25 to 0.5 mg/kg of body weight. Greenman says IM ketamine peaks around five minutes.
- Oral ketamine. A standard dose is 1 mg/kg of body weight. Greenman says oral ketamine effects peak at about 15 to 30 minutes.
- Ketamine lozenges. Greenman says this is a less invasive option for patients to do the treatment at home, but less medication will be able to enter the bloodstream. Standard dosing varies.
- Intranasal ketamine (Spravato). As this is the only FDA-approved formulation of ketamine for depression, there is standard dosing. The dose for TRD is 56 mg for adults, which may increase to 84 mg. For major depressive disorder or suicidal ideation, the dose is 84 mg for adults. For nasal administration, medical providers give patients a nasal spray device, similar to one you might use for a stuffy nose. Greenman says peak effect of intranasal ketamine is around 15 minutes.
Spravato is usually recommended for at least six months. But if considered effective, your provider may recommend you take the medication long term. Since the other forms of ketamine are off-label, there aren't regulated treatment durations. Your doctor may recommend you have more ketamine treatments in the beginning, and then have the treatment less often as a maintenance therapy. Treatment duration and frequency depend on the discussion between a patient and their medical provider.
Ketamine Benefits
Using ketamine for depression has a few key benefits:
- Rapid onset. Koo says that other medications would take four to six weeks to achieve remission, whereas ketamine is going to be much faster.
- Relief from depression symptoms. Especially with TRD, other treatments may not be working. Ketamine may be the treatment to finally provide relief from depression.
- May be combined with psychotherapy. Because ketamine can induce an altered state of consciousness, individuals may be more receptive to emotional processing and therapy.
Ketamine Side Effects and Risks
Using ketamine for depression also has side effects and risks:
- Medical surveillance is needed after treatment. All patients require some level of medical surveillance after treatment, like staying in the clinic so the staff can watch vital signs and assess for loss of consciousness. Koo also says that patients cannot drive post-session for at least 24 hours.
- Dissociative effects. The effects differ between individuals, but some may experience emotional numbness or detachment, out-of-body experiences or hallucinations. Koo adds that these effects can be uncomfortable ketamine side effects for many people.
- Nausea. Nausea is one of the most common side effects, and usually, the side effect is mitigated with medications prior to treatment.
- Headaches. Headaches are another common effect, also treated with medicine beforehand.
- Abuse potential . Proper screening and ongoing monitoring are essential with ketamine administration. It’s vital that people work with licensed psychiatric clinicians who can prescribe appropriately and watch for signs of misuse or dependence.
Is ketamine addictive?
Dr. Leonardo Vando, the Maryland-based medical director of Mindbloom, a platform that provides services to affiliated psychiatric medical practices in more than 35 states, says that ketamine is "not physically addictive in the way that substances like alcohol and nicotine are. However, it is possible to become psychologically dependent on ketamine – especially when it is taken without proper clinical supervision."
Are there ketamine withdrawal symptoms after treatments end?
When ketamine for depression is taken under medical supervision, withdrawal symptoms are less common. The dosage of ketamine administered is not meant to induce physiological dependence.
When ketamine is abused, American Addition Centers cites common symptoms may include:
- Drug cravings
- Mood swings
- Heart palpitations
Who Is Eligible for Ketamine Therapy?
Ketamine therapy is usually for individuals with depression who have not responded to other types of treatment or those with active suicidal thoughts.
Beyond that, anyone considering ketamine therapy would need additional medical clearance. This process includes:
- Patient intake. Your provider will take a complete medical history, family history , surgical history, medication list and allergies.
- Rule out contraindications. Your provider will need to make sure you don't have a condition that makes taking ketamine unsafe, like pregnancy, heart disease , uncontrolled high blood pressure, untreated thyroid disease, schizophrenia, acute drug intoxication or acute mania.
- Psychological assessment. Greenman says she checks for risk of abuse or active substance use disorders or other mental health conditions that could interact with ketamine, like psychosis.
- Assessment of developmental and trauma history. Greenman wants to understand what her patients have tried for previous treatment, their religious or spiritual preferences and their support system at home.
- Informed consent. Everyone needs to sign consent forms and agree that they understand the risks and benefits of ketamine therapy and the importance of regular medical follow-ups.
Does Insurance Cover Ketamine?
Sultan says that because ketamine is often used off-label, it's difficult to get any insurance coverage. He adds that some ketamine providers offer financial assistance programs to help patients pay for treatments.
"Advocacy groups and health care professionals are actively engaged in efforts to promote greater access to and affordability of ketamine treatment," he explains.
With continued research on safety and efficacy, insurance coverage may improve.
Understanding Male Depression

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Greenman is a functional medicine physician and head of ketamine-assisted psychotherapy at Blum Center for Health in New York.
Koo is the founder and chief medical officer at Neuro Wellness Spa. She is board-certified in psychiatry and addiction medicine. She is also a medical director and clinical supervisor at Clear Recovery Center and is on the board of directors of the Clinical TMS Society. She is based in Manhattan Beach, California.
Sultan is a teaching psychiatrist, research scientist and the director of Mental Health Informatics at Columbia University Irving Medical Center/New York State Psychiatric Institute in New York.
Vando is based in Maryland and is the medical director of Mindbloom, a platform that provides services to affiliated psychiatric medical practices in more than 35 states.
Lavretsky is a professor of psychiatry in-residence at the David Geffen School of Medicine at UCLA. She’s also director of the Late-Life Mood, Stress and Wellness Research Program and director of the Integrative Psychiatry Clinic.
Tags: mental health , depression , drugs , psychology , psychiatry
Most Popular
Patient Advice

Best Hospitals

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
Get a second opinion.
Paul Wynn Aug. 22, 2024
How Chemotherapy Works
Payton Sy Aug. 20, 2024
What Is Bariatric Surgery?
Claire Wolters and Christine Comizio Aug. 19, 2024
Medicare Coverage: Alternative Medicine
Christine Comizio Aug. 16, 2024

Barbara Sadick Aug. 14, 2024

Reduce Health Care Costs in Retirement
Elaine K. Howley Aug. 12, 2024

Using Medicare’s Telehealth Coverage
Elaine K. Howley Aug. 9, 2024

9 Screenings to Lower Medicare Costs
Elaine K. Howley Aug. 7, 2024

How SHIPs Can Help
Payton Sy Aug. 7, 2024

Preparing for Surgery
Ruben Castaneda and Christine Comizio Aug. 7, 2024


Should You Try Ketamine Therapy?
6 questions to ask yourself before trying ketamine therapy..
Posted August 16, 2021 | Reviewed by Devon Frye
- What Is Ketamine?
- Take our Depression Test
- Find a therapist to overcome depression
- Ketamine is a dissociative anesthetic that is thought to improve the brain's neuroplasticity and was legalized for therapeutic benefits.
- Ketamine has also been found effective in combating treatment-resistant depression, PTSD, and anxiety.
- Ketamine is not 100 percent effective and is usually rather expensive (at least several hundred dollars a "session").
- Ketamine therapy is as much (if not more) about the “therapy” than it is about the “ketamine.”
If you clicked on this headline, there’s a good chance the answer to your question is: possibly! Ketamine is safe and effective. If a passive-aggressive colleague sent you this link, maybe the cure for your problems is to move desks. If you googled this question, make sure the article you're reading isn't posted by a ketamine therapy clinic because, and you'll never believe this: they have an incentive for you to try ketamine therapy .
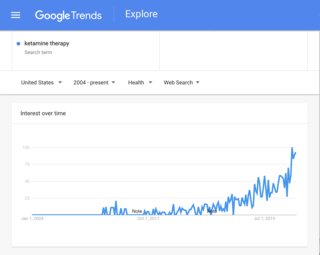
There has been a marked increase in exposure and interest for this novel therapy, as you can see in the Google Trends chart here. Ketamine has been in a state of heightened media frenzy ever since the FDA approved the ketamine-derived nasal spray Spravato for treatment-resistant depression in March of 2019. Since then, ketamine has been investigated as a helpful treatment for depression, PTSD , anxiety , and slow news days. Recently, there was a major scientific breakthrough in understanding ketamine’s mechanism of action . Last month, Field Trip, a chain of ketamine clinics, was listed on the Nasdaq. Plus, ketamine clinics have been popping up like Starbucks in major urban areas.
Ketamine is a safe and effective form of therapy and, possibly, the first proverbial “drip” in an eventual waterfall of psychedelic-assisted therapy options. Regardless, it's a watershed moment for this novel therapy.
What Is Ketamine Therapy?
Ketamine is a dissociative anesthetic, considered by some to have psychedelic properties. It is thought to affect the glutamate neurotransmitter in the brain, improving neuroplasticity and interrupting ruminative patterns such as those found with depression. Ketamine therapy entails an intake session with a therapist, then several “sessions” in which ketamine is administered, then integration and follow-up meetings with a therapist. Ketamine can be administered through nasal sprays, lozenges, intramuscular injections, or intravenous infusions.
So the question remains: should you try it? To answer that question, here are 6 others:
What’s Bothering You?
If you have treatment-resistant depression, then this treatment might break through that resistance. Ketamine has also been found effective in combating PTSD and anxiety.
If your depression isn’t “treatment-resistant” because you have yet to treat it, you may want to consider conventional antidepressants first. They have been studied more and longer than ketamine has been studied. Plus SSRIs are likely less expensive. However, they take weeks to start working, if at all. They’re only about 20 percent more effective than a placebo and they come with their own lengthy list of side effects.
Ketamine is both short-acting and fairly long-lasting. What does that mean? It means that the effects are felt within minutes and may last for a week to a month. One 2019 study found the heightened effects of ketamine started within minutes and lasted for at least a month after the session. But a different study from that same year found that the effects of a placebo and conventional antidepressants caught up to ketamine’s effects after seven days. So there is a range. But it’s a safe bet that ketamine offers some bang for your buck—if by “bang” you mean fairly stable relief from mental anguish.
If, however, you have ever suffered from psychosis , schizophrenia, mania , or paranoia , please be aware that ketamine may not be for you. There’s a reason ketamine has been considered a “ schizophrenomimetic .” That’s not just an award-winning spelling bee word, it’s the name for a drug that can mimic schizophrenia-like mental conditions.
Are You Prone to Addiction?
You might think that an affirmative response to this question would preclude you from being a good candidate. But in fact, ketamine may actually be a good treatment for addiction . Two clinical trials showed that ketamine reduced the chance of relapse for cocaine addicts and alcoholics. Ketamine has shown positive results in treating nearly every kind of addiction—except for addictions to ketamine, of course. (Shockingly, the treatment for ketamine addiction is not more ketamine.)
How Risk Intolerant Are You?
Currently, there are no long-term studies about the effects of ketamine as opposed to many conventional antidepressants. Also, ketamine is not 100 percent effective. But then again, literally no treatment is 100 percent effective at curing depression—except perhaps puppies (but this is personal conjecture as no clinical studies have been done yet).
There are also some concerns over risks to the liver, bladder, and kidney . Ketamine can increase heart rate and blood pressure. So people with issues like hypertension may want to steer clear. It’s really a question for your primary care doctor, not an internet blogger, no matter how informative and entertaining she might be.

Are You Afraid of Needles?
Intravenous Infusions are by far the most commonly used and most commonly studied method for administering ketamine. This is because the dosage can be extremely carefully controlled and the journey can be stopped at any moment. The drip controls the trip.
Intramuscular injections are delivered into the thick muscles of your arm, hip, thigh, or if you want the real veterinary clinic feel, the buttocks. With IM infusions , ketamine is administered all at once and cannot be titrated down once injected. IM infusions cannot be as easily mixed with medicines to combat nausea and increased blood pressure.
There are also lozenges and Spravato, the nasal spray which uses esketamine , to consider. Both are administered under supervision (either in an office or remotely on Zoom). These are cheaper alternatives since they do not require special equipment nor a physician trained in anesthesiology. They’re also convenient since patients may even administer the treatment at home themselves. However, both provide relatively lower dosage than the infusion route due to imprecise administration.
Whichever method you’re considering, by far, the most important part of the process is the role played by a mental health professional. Whether this is a psychiatrist, therapist, or integration coach, make sure this is an individual you feel safe around.
How Much Are You Willing to Spend?
Take a deep breath. Assuming you don’t have a chronic pain syndrome, there is a very high chance that insurance will not cover ketamine therapy. Infusions may set you back several thousand dollars but it will include a half dozen infusions sessions, an intake, integration sessions, and follow-ups. The nasal spray Spravato can cost from $590 to $885 per treatment session. But how many treatment sessions are needed is up for debate. Lozenges (administered in the office or monitored remotely over Zoom) can cost about a thousand dollars for 1-6 sessions depending on where you go.
All of the options have a range but all will cost at least several hundred dollars. Unfortunately, the field is new and speculative and therefore, draws many hucksters. Make sure to take time to research your clinic and read any reviews if available.

What Else Should You Know?
Ketamine therapy is as much (if not more) about the “therapy” than it is about the “ketamine.” Make sure you’re working with a clinician you trust and make sure to see an integration therapist with whom you share a connection. Integration is the process of talking with a therapist after a psychedelic or psychoactive session in order to glean meaningful therapeutic insight. Ketamine is a novel and exciting part of the treatment but it’s the therapy that can really lead to lasting change beyond the neural rewiring.

Sarah Rose Siskind is a science comedy writer based in New York City.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Ketamine’s Catch-22
The drug has a hard-partying past—and a promising future in treating depression.
/media/cinemagraph/2024/08/21/03_Ketamin_animation_R8Article.mp4)
Last week, five people were charged with providing the ketamine that led to actor Matthew Perry’s death. It’s the latest news in a saga that has renewed questions over ketamine’s dual role as a promising depression treatment and an illicit drug.
Questions about ketamine are now all the more relevant because of a pandemic-era decision that allows doctors to prescribe the drug online—transforming the way Americans access and maintain prescriptions for controlled substances.
What role does ketamine have to play in the future of depression treatment now that the prescribing landscape has changed?
This is the third and final episode of Scripts , a new three-part miniseries from Radio Atlantic about the pills we take for our brains and the stories we tell ourselves about them.
Listen to the story here:
Subscribe here: Apple Podcasts | Spotify | YouTube | Overcast | Pocket Casts
The following is a transcript of the episode:
Hanna Rosin: This is Radio Atlantic . I’m Hanna Rosin.
Today we have the third and final episode in our series exploring psychotropic meds and the cultural stories surrounding them. In those early, uncertain days of the pandemic, the government made a decision—a decision that is proving very hard to walk back and that transformed how we access these drugs, how doctors prescribe them, and how we stay on them.
This week, a story about ketamine and about the fallout of that decision. Reporter Ethan Brooks will take it from here.
Ethan Brooks: Okay, I’m going to start with this doctor. His name is Scott Smith, and his story starts back before the pandemic. Smith is working in Mount Pleasant, South Carolina, as a family doctor—so sick kids, high blood pressure, all sorts of things.
One day he’s driving to work, listening to the radio, and NPR is airing a story about ketamine as a treatment for depression.
Scott Smith: And as I was driving to work and I heard them talking about that, I said out loud, That’s the dumbest thing I’ve ever heard of. Ketamine would never help anybody for depression .
Brooks: You said that out loud?
Smith: Yeah, to myself as I was driving because it just was ludicrous.
Brooks: This felt ludicrous because, for Smith, that’s just not what ketamine was for. For him it was as an anesthetic, something you might give to a kid who needs stitches on their tongue, get them to quit squirming. The way it functioned, as he understood it, was to separate the mind from the body.
For other people, ketamine is a party drug, going by names like K, Special K, and, according to the DEA, “Super Acid.” I haven’t heard that one before.
But recently, ketamine’s new gig is as a depression treatment, and a promising one—promising because it works fast, which is a useful feature for people who are suicidally depressed. And it works well for patients for whom other depression treatments don’t work.
Ketamine for depression is often prescribed off-label. And in 2019, the FDA approved an on-label treatment called Spravato, which is a nasal spray. It’s the first genuinely new, FDA-approved depression treatment in 50 years.
After Scott Smith heard that story on the radio, he did some research. And before long, he was a believer.
Smith: I asked myself, Wait a minute. Why has nobody told me about how powerful this treatment is? And why isn’t this being used?
Brooks: So Scott Smith, when he learned all this, felt, in a way, offended that we had been sitting on this drug for so many years, that so many people, including people really close to him, had been struggling with severe depression and that ketamine wasn’t an option that was available to them.
Smith: It was in my face that this was real, and I couldn’t deny it. I couldn’t deny it. To deny it, to me, would mean being a bad doctor. This situation had been presented to me by the universe. My best friend killed himself.
There was no way I was going to let this pass by.
Brooks: Have you felt that before? Like, is this the first time that’s happened?
Smith: That was the first time it overwhelmed me.
Brooks: Smith wanted to get ketamine to as many patients as he could who needed it. So he made a bold decision: He starts his own practice, one that serves both ketamine patients and his normal family-practice patients. He rents an office with two completely separate waiting rooms, so you could be sitting in one waiting room and totally unaware that the other exists. The sign on the door to the first waiting room said smith family, md. The sign on the door to the other room said ketamine treatment services. Scott Smith was behind both doors.
The practice did well. Patients filled up both waiting rooms. And maybe Smith would have liked to treat more patients, but it was a brick-and-mortar office, so that was that. And then the pandemic came, and everything changed.
Okay, so it’s March 20, 2020. To set the scene, this is nine days after the World Health Organization declared COVID-19 a pandemic. This is the same day Governor Cuomo issued a stay-at-home order for all New Yorkers, United announced it will cut down international flights by 95 percent, and the DEA made an announcement: Given the circumstances, doctors no longer had to see patients in person—at all—to prescribe controlled substances.
And this decision, I’d like to submit, is among the most enduring and consequential policy decisions of the pandemic. Before this change, with few exceptions, if you wanted a controlled substance—amphetamine, Suboxone, ketamine, Xanax, testosterone—you needed, at some point, to see a doctor in person.
After the March 2020 change, that in-person barrier was gone. It became easier to get prescribed and easier to stay prescribed. And this, especially in a pandemic, saved lives. But something else happened, too.
The way we access and maintain medications underwent a fundamental shift. The new policy brought us into a new era, one where patients have a lot more power—the power to diagnose and treat ourselves without leaving the room.
Brooks: From 2020 to 2022, one study found a tenfold increase in telehealth visits. Americans, as we’ve discussed, started taking a lot more psychiatric medications, and the worlds of venture capital and startups saw an opportunity: psychiatry at a scale that would have been impossible before. The money poured in, and before long, the environment resulting from this confluence of demand, policy, and money had a name.
I’ll just read a few recent headlines here: “New Mental Health Clinics Are a Wild West,” “Adult ADHD Is the Wild West of Psychiatry,” “The Wild West of Online Testosterone Prescribing,” “The Wild West of Off-Brand Ozempic,” “The ‘Wild West’ of Ketamine Treatment.”
You get it—a Wild West, a new world of access and autonomy for patients and for doctors. So Scott Smith—half family-medicine doctor, half ketamine doctor—sees these changes and decides to go west.
Smith: I went all in. I went all in. I became licensed in 48 states.
Brooks: Smith closes the office with two waiting rooms and builds a new practice from the ground up. Now he would only provide ketamine treatment, mostly in the form of off-label, low-dose ketamine lozenges.
Smith: In this practice, every single patient is being treated with the same medicine. The treatment protocol that we’re giving these patients is the same, for every single patient.
It’s like a Baskin-Robbins store that only serves vanilla ice-cream cones. How fast would a Starbucks run that only sold coffee with cream and sugar? That’s it.
Brooks: I started pointing out to Smith that comparing ketamine, a Schedule III controlled substance, to ice cream or to coffee with cream and sugar might give the wrong impression.
And as he clarified his vision, I realized it wasn’t “drugs as candy” that he was really going for or treatment as fast food. What he had in mind was all the things fast-food restaurants do well: efficiency, specialization.
And in a country where someone dies by suicide every 11 minutes, maybe fast-food-style efficiency, applied to a fast-acting depression treatment, isn’t so bad.
Brooks: In Smith’s practice, the problem could be PTSD, anxiety, depression. The solution would be ketamine, ketamine, ketamine.
Smith: I was taking care of about a thousand patients in a pool and, at the peak, it was around 1,500 patients.
Brooks: The more I talked to Smith—and for reasons that will become clear a bit later—I wanted to know: Who were Smith’s 1,500 patients? I also wondered if his patients might be more into the “Super Acid” side of ketamine than the depression treatment.
After all, ketamine can be dangerous. There’s an FDA warning that includes stuff like urinary tract and bladder problems. But also; respiratory depression.The autopsy for Matthew Perry, who played Chandler Bing in Friends , determined that he died from the “acute effect of ketamine.”
I started calling Smith’s patients just a few months after Perry’s death. And I want to just introduce you to two here.
Willow: Good afternoon.
Brooks: Willow, a nurse in Tennessee. I’m going to use a nickname to protect her privacy.
Johannah Haney: Hi. This is Johannah.
Brooks: And Johannah Haney, a writer in Boston. And I want to tell their stories because they help explain the profound positives that came with the 2020 rule change and, also, the risks inherent in that new Wild West.
Haney: Nobody starts with ketamine treatment, you know what I mean? It’s just like, this is sort of the last stop.
If I wasn’t going to get relief, I just wanted it to be over and done. And if you think about being on an airplane, and you’re just so restless, and all you want is to be at this final destination, and, you know, you’re uncomfortable, and you’re bored, and you’re just like—you know that feeling that you get on a plane? It’s how my life felt to me.
Brooks: Johannah had been struggling with depression for years, had tried all the usual depression treatments—SSRIs, anti-anxiety medications, antipsychotics—some of which would work for a while, until they didn’t.
There was one that did work well for her.
Haney: But it was affecting the muscles in my mouth. So as time wore on, you couldn’t understand my speech anymore, which was kind of a big problem.
Brooks: Willow, the nurse, struggled with the usual depression meds, too.
Willow: I tried Prozac. I tried Paxil. I tried Wellbutrin. And nothing was working.
I no longer went to church. I couldn’t seem to even answer phone calls from my friends. I would just lay in bed. I couldn’t even make myself brush my teeth. I’ve had plenty of dental work done since to try to reverse some of the damage. There was no sort of existence other than me just fighting against taking my own life.
Brooks: Had you experienced anything like that before?
Willow: I haven’t.
Brooks: Nothing was working for Willow until, one day, she found some research on ketamine.
Willow: At that point, I felt like, What do I have to lose? It couldn’t get worse than what it was.
Brooks: Johannah and Willow liked Dr. Smith. Johannah, through her screen, found him to be warm and attentive. Smith prescribed them lozenges to be dissolved in their mouths. The lozenges were supposed to taste like cherry or raspberry, but mostly they tasted bitter, waxy. What the patients hoped for wasn’t a cure; that didn’t seem realistic. What they hoped for was a separation from the needling idea that it might be better to not be alive.
And there were all sorts of separations that needed to be delicately managed: Depression separated them from the things and people they loved in life. The ketamine separated their minds from their bodies, sometimes so much that it was scary, sometimes so little that they felt nothing. But the only separation that mattered was between two parts of their minds—one that sought normalcy and one that sought nothingness.
Willow: Within the first few doses, there was a drastic difference. It wasn’t like I was able to leave my house or I was even able to clean or do things such as that yet, but I would actually get in the bathtub.
I actually was able to hold my concentration for a little bit. Because I was just having constant anxiety attacks.
Haney: I started doing the dishes, which is something that I really couldn’t do before. So I still felt like garbage, but I could do the dishes.
Willow: Within a month, I was out my house, checking my mailbox. And about two or three months later, my kids felt like they had their mom back.
I got a promotion at work within about six months, and almost a year later, I was thinking, Well, I’ll go back for my next degree . So it made all the difference in my life.
Brooks: Here were two patients, Willow and Johannah, finally finding treatment that worked—treatment that would otherwise be too far away or too expensive. They were patients reaping the full benefit of ketamine’s so-called Wild West.
When we come back: the costs.
Brooks: Okay, so before we get back to Willow and Johannah and Dr. Smith, I want to move forward in time a bit, around three years after the 2020 change that opened up remote prescribing for controlled substances.
In the three years since the prescribing rules changed, the world changed. There was a nationwide Adderall shortage, driven, in part, by a flood of new telehealth patients. And Scott Smith wasn’t the only one with the idea to make a national, online ketamine practice. Startups with names like Joyous and Mindbloom have served thousands of patients.
And the DEA, looking at all of this change, thought, Okay, maybe things have gotten a little out of hand .
So in February 2023, they proposed a new set of rules: not to go back to exactly how things were before the pandemic, but a rule that would force most patients to see doctors at some point, in person. So in February 2023, those new rules went online for public comment. A month passed and, in that time, the DEA received more than 38,000 comments—a record number.
I’ve read thousands of those comments, downloaded them into one huge spreadsheet, and if you read them together, it’s kind of an extraordinary document—story after story about how this new access, new autonomy changed people’s lives.
The comments are from patients, doctors, pharmacists, trans people who need testosterone, Marines who need testosterone, polio survivors, palliative-care patients, teenagers, and octogenarians.
They talk about how virtual access to these drugs is a matter of life or death. Some wrote long stories. Others, writing about the new, more restrictive rules, were more direct, like, quote, “This is a horrible idea.”
There are so many comments, it’s almost easier to get a real picture of it through the search bar. The phrase “saved my life” appears 444 times—all in all, a coalition of suffering people come to deliver one message: That Wild West, it suits us just fine. We didn’t choose it then, but we’re choosing it now. We want to stay in that Wild West, come what may .
The DEA listened. On May 9, 2023—a couple months after they proposed those new rules—the DEA said, Never mind. We’ll keep the 2020 emergency rules in place. We’ll try again a bit later . And until then, it’s the Wild West—for better or worse.
On May 9, 2023—the same day the DEA announced it would back off on its new rule—Willow, the nurse, got an email from Dr. Smith.
Brooks: Do you remember where you were and what you were feeling at that time?
Willow: Yes, I do. I had just seen him the day before, and so I couldn’t believe it.
Brooks: The email informed his patients—all of them—that his practice would shut down immediately.
Willow: I panicked. I didn’t want to go back to where I had been before.
I realized I needed to use my brain while it was still functioning okay and hurry up and find help.
Brooks: Like a ticking clock, sort of. Like there’s a countdown.
Willow: It was, and it was very scary. I didn’t want to become suicidal again. I don’t want my kids to lose their mom. I enjoy helping people with my job. I didn’t want to slowly just kind of disappear into nothing.
Smith: Well, on May 9, I got done seeing patients in the morning. I was in my office doing paperwork, and there was a banging on my front door, like somebody was just going to knock my front door down. So I went down there, and it was two big, male DEA agents with guns on their hip, and they said, Can we come in? I said, Why?
Brooks: The agents were there with an order. The order says that over about a four-year period, Smith issued around 2,224 prescriptions for controlled substances in states where he either was not licensed or failed to consult state drug-monitoring programs.
It ordered him to stop prescribing ketamine—or any other controlled substance, for that matter.
Smith: It just felt like the end of the world. It just felt like the end of the world. I felt like, Am I crazy? Am I a bad doctor? Did I really do everybody wrong? And then, for a long period of time, I would just fluctuate back and forth between that.
Brooks: With regard to the state drug-monitoring programs, Smith maintains he did everything correctly. As for the illegal out-of-state prescriptions, he says all these patients either traveled to visit him in person or traveled to a state where he was licensed to consult with him via telemedicine.
And around the same time Smith’s practice shut down, that same story of sudden loss of treatment was happening around the country. Ketamine Wellness Centers, a brick-and-mortar chain, shut down in March 2023 due to funding issues. Patients, some of them suicidally depressed, lost access to treatment immediately. Babylon Health, a telehealth startup once valued at $4.2 billion, was sold off for scraps. And Cerebral, another multibillion-dollar startup treating depression, insomnia, and ADHD, came under investigation by the Department of Justice for violating the Controlled Substances Act.
Patients were forced to find new providers. Whatever the cause, the result for patients was the same: instability and a lot of very tough decisions.
Haney: I mean, I have legitimately and recently thought, like, I’m just going to go back on that one drug that worked for me .
Brooks: For Johannah, that was the antipsychotic medication that worked for her depression but interfered with her ability to speak.
Haney: Honestly, I’m like, Would I rather feel good or be able to talk?
That’s sort of where my mind is. Like, I may rather just take that and let my mouth muscles do what they’re going to do. So I’m not going to be able to talk anymore. I’ll write things down.
Brooks: It sounds like it feels kind of clear to you that it would be worthwhile, if you had to, to kind of go back to having problems with speaking or not being able to speak in order to feel okay.
Haney: I think for sure. Yeah.
Brooks: Willow, after Smith shut down, struggled to find another provider. So when Smith stopped, she stopped. Life got harder again. But a few months later, she found another doctor online and started back on ketamine again.
Willow: I forget what month I’m on. I’m slowly kind of coming back up. I don’t need a large dose. I really just need a smaller dose and, also, I don’t need it as often anymore.
Because I want to take it as infrequently and at the lowest dose absolutely possible.
Brooks: Why is that?
Willow: It just kind of makes me feel better because I’m scared. I’m scared that it could be taken away again. And what if I can’t get my medicine to function? I never had that fear before of having a lifesaving medicine just be taken away like that.
Brooks: Got it. So just to make sure I understand correctly, you could try to take it more consistently or at a higher dose and maybe get back to feeling normal and energetic and kind of back to where you were at the best of the Smith times, but at the moment are kind of intentionally not doing that, as to not become too reliant, because the medication’s at risk. Is that right?
Willow: Yes, sir. I’m just really scared of it being taken away again and what happens if I go back to how I was. That’s not a life. That’s not a life at all.
Brooks: Trade-offs are a part of medicine: effects and side effects. It comes with the territory. Even Johannah’s trade-off—her mood for her ability to speak—that’s part of the usual equation, just an extreme example.
But for Smith’s patients and others who have had to navigate the uncertainty of this moment, it’s different. This Wild West can keep patients from sticking with treatments that work for fear of them being taken away—a Wild West not so much for its lawlessness or its dangers but for its uncertainty, the feeling of being surrounded by the unknown.
The DEA has said that it will come back in the fall of 2024 with new, final rules for how we access controlled substances online. And in some ways, that feels like an opportunity—or maybe just a moment—not just to reset policy but to strip away some of the stories, preconceptions, shorthand that surround so many of these drugs.
The policy part is probably easier. There are a lot of people arguing for a special registry of virtual prescribers—ones that are known to be reputable, issuing proven treatments—a system that would protect patients from bad actors without ending access to virtual-only care.
But resetting narrative, stripping away stories built up over decades—that is a more complicated proposition. Maybe it starts by just acknowledging what we know and don’t know about how these drugs work in our bodies and, when we start on a drug, having a lengthy discussion of what it might take to stop.
That, at least, is somewhere to begin.
Brooks: Scripts is produced and reported by me, Ethan Brooks. Editing by Jocelyn Frank and Hanna Rosin. Original music and engineering by Rob Smierciak. Fact-checking by Sam Fentress. Claudine Ebeid is the executive producer of Atlantic audio, and Andrea Valdez is our managing editor.
If you’re having thoughts of suicide, please reach out to the national suicide-prevention lifeline at 988 or the Crisis Text Line. For that, you text “talk”— T - A - L - K —to 741741.
Radio Atlantic will be back next week.
About the Author
More Stories
A Dangerous Idea About How the Brain Works
The Drug That Could Help End the Opioid Epidemic
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Health and Wellness
What a Ketamine "Trip" for Depression Is 'Really' Like
Treating depression with the former party drug is a major development in psychiatric medicine, and now you can even do it from the comfort of your home.
Chelsea Greenwood is an award-winning writer and editor with a focus on lifestyle content at renowned local, regional, and national outlets — both in print and online. She has more than 15 years of experience in journalism, backed by her journalism degree from the University of Florida. She is currently a developmental editor for The Spruce and MyDomaine as well as a news editor at Static Media's The List. In additional to InStyle, she has also written for Teen Vogue, Self, Vice, Vulture, Business Insider, Apartment Therapy and more.
:max_bytes(150000):strip_icc():format(webp)/Chelsea-Greenwood-2000-874cd3999d2f45acbbdb064e34243a8a.jpeg)
Leaving the house before the pandemic was hard enough, thanks to my social anxiety and depression. But once lockdown started? Forget about it. Being in quarantine exacerbated my symptoms until, one day, I realized that I could hardly get out of bed. From eating and working to binge-watching and texting, I did it all in my bed.
I was on antidepressants, and my depression was worse than ever.
While I'd heard good things about ketamine therapy, I figured it was too pricey, and the idea of going to an actual brick-and-mortar clinic was beyond me in my depressed state. But Google was onto me: I was served an ad for Mindbloom, an at-home ketamine treatment company.
When I looked it up, the cost was considerably less than I had expected (even though the company doesn't take insurance), and I read that dedicated "guides" would be there via video chat to help me along the way and process my experiences. So, after some more research, I signed up. What did I have to lose?
As it turned out, a lot. Over the past 12 weeks and 12 treatments, I've lost that heaviness that kept me stuck in bed like gravity. I lost that ever-present sense of impending doom. Plus, I found a little bit of clarity and a lot of hope. Things aren't perfect — I still have good days and bad — but I feel like I'm at the beginning of a season of change, full of possibilities.
I'm not alone. More and more depression sufferers who haven't found adequate relief via conventional methods are turning to ketamine therapy, and treatment clinics are popping up across the country. To explain what exactly the drug does to your brain and its potential for treating mental illness, I turned to two experts in the field for their input.
What is ketamine, exactly?
Although it was first discovered in 1956 and used as an anesthetic for animals, ketamine was cleared by the FDA in the 1970s as a human anesthetic. Since then, it's been used extensively to sedate patients for surgery, including soldiers injured in the line of duty during the Vietnam War.
In addition to sedation, the trance-like state ketamine produces comprises pain relief; amnesia; and a sense of dissociation, like you're outside of your body. Taking a high dose of ketamine may lead to a psychedelic experience known as a k-hole, involving severe dissociation, intense visual hallucinations, and feelings of unreality.
How does ketamine help treat depression?
So, when and why did researchers first begin testing ketamine as a treatment for depression? Well, at the start of the 21st century, ketamine was found to have potent and rapid antidepressant properties at sub-anesthetic doses, explains Ryan Yermus, M.D., co-founder and chief clinical officer of Field Trip Health , which provides ketamine therapy for depression. "While the most commonly used medicines, selective serotonin reuptake inhibitors (SSRIs), generally require weeks of continual dosing to achieve a response (and even then approximately one-third of patients will not respond after two or more courses of treatments), ketamine provides a safe, more rapid-acting treatment for depressive conditions," he says.
Although more research needs to be done on what exactly ketamine does to the brain, Gerard Sanacora, M.D., Ph.D., a Yale Medicine psychiatrist and a professor at the Yale School of Medicine, says that evidence suggests the drug alters the brain's adaptive capabilities — almost like rewiring it. The brain's ability to change both structure and function throughout one's life is called neuroplasticity.
"The synapses, the connections between cells in the brain, appear to be changing more rapidly shortly after treatment with ketamine," Dr. Sanacora says. "We believe this can influence a person's ability to change thought and behavior patterns that are associated with depression."
That's why ketamine treatment doesn't just hinge on the drug itself. It typically involves therapy and integration work, too: putting the mental and emotional revelations you experience during treatments to practical use in your daily life (e.g., starting a new meditation practice, creating a daily exercise ritual, etc.) during a time when your brain is in this state of change.
How significant of a development is ketamine as a treatment for depression?
"The discovery and development of ketamine for the treatment of depression has dramatically altered the way we think about depression treatment," says Dr. Sanacora.
On top of providing hope for those with treatment-resistant depression, the use of a drug not previously intended for psychiatric treatment has had a profound effect in the field of mental illness treatment. "This has led to a whole new wave of exploration in attempts to develop new and improved treatments for depression and other related neuropsychiatric disorders," Dr. Sanacora says.

So, is it legal?
Yes, but the law is not so cut and dry. Currently, ketamine is approved for clinical use as an anesthetic, explains Dr. Yermus. When a drug is prescribed for uses other than its original intended function, it's being used off-label.
"Using medicine off-label is very common in practice as doctors learn that safe medicines can be effective for other purposes, and the use of ketamine in mental health is just one of many examples," he says. So, if a doctor prescribes you ketamine for the treatment of depression or anxiety off-label, it is legal and safe.
However, in 2019, the FDA approved one form of ketamine, a nasal spray called esketamine (brand name Spravato), to treat depression — a promising step forward in this field of medicine.
But ketamine is still a controlled substance, so it's illegal to possess without a prescription.
What are the different ways you can take ketamine?
For therapeutic purposes, ketamine can be taken via intramuscular (IM) injection, intravenous (IV) infusion, orally (as a tablet), or nasally (as a spray). More research is needed to determine which method is the most effective. Generally, only the tablet, like the kind I take, is self-administered (i.e., taken at home), and the rest are administered by professionals in a clinical setting.
What does a ketamine treatment session feel like?
While everyone's ketamine treatment session will differ, many describe the experience as a euphoric, dreamlike state in which the world around them seems to fade away, everyday cares dissipate, unusual thoughts emerge, and vivid memories come to the surface. Some mild visual hallucinations are possible.
The psychedelic experience is intended to be gentle, not scary. Depending on the dosage, the length of the treatment will vary, but most sessions take anywhere from 40 minutes to two hours.
Here's what my first ketamine "trip" looked like:
Per the instructions, I didn't eat for four hours before my treatment. There's potential for nausea when taking ketamine, so Mindbloom provided me with anti-nausea medication, which I took one hour before I began my treatment.
When it was time to begin, I tucked the ketamine tablet inside my lip to let it dissolve. I swished it around with my saliva to help it absorb into my bloodstream, and then I spit the rest out. I turned on a zen Mindbloom playlist, put on an eye mask, and laid down in bed to let the trip begin.
Mindbloom encourages you to set an intention before each treatment — something that's not quite a goal but perhaps a question you want answered or a topic you want to explore. Mine was finding joy. As the session began, I felt a strong need to connect to something deeper and more powerful than myself, something spiritual (I consider myself an atheist). Then I saw an image of myself as a child. My first instinct was to fold her in my arms and protect her from everything to come in life. It made me weep.
Behind my closed eyes, I saw some mild visuals of swirling shapes and colors. I never felt scared or overwhelmed at any point — simply like I was floating down a river and observing thoughts, feelings, and memories as they passed by. I felt euphoric and slightly detached from my body, which felt somewhat tingly and numb, but I was still aware of the room around me.
Overall, you're supposed to dedicate one hour to your treatment. I found that the ketamine kicked in about 10 to 15 minutes after taking it, and then I would have about 40 minutes or so of the "trip" experience. Directly afterward, Mindbloom encourages patients to journal what they saw, felt, and experienced so they can later process it.
I felt a little groggy after my first session, but generally didn't feel any other side effects from taking the ketamine. My guide told me that this is a very "clean" way of taking the drug in that it produces very few side effects, if any.
How long does it take to work?
Like with most psychiatric medicines, your mileage may vary. While some see improvement in their depression symptoms immediately after the first treatment, it doesn't usually last, Dr. Sanacora says. Research indicates that ketamine therapy has a cumulative effect.
"Most people require a series of treatments in order to improve the chances of sustaining the response," he says. "Many of those people then also require some ongoing maintenance treatments every couple of weeks or monthly to keep the depression at bay." He notes that there are active research studies trying to find ways to extend this response, but there are no clear methods of achieving it at this time.
Dr. Yermus agrees that the timing depends on the person. "The severity of the condition is generally a guide for how many sessions people need — so someone with debilitating, acute depression will likely need more sessions than others with more moderate symptoms," he said. "Clients with mild anxiety and depression who feel stuck and disconnected can sometimes have a profound 'aha' moment after one or two sessions."
Personally, I had some significant revelations during the first couple sessions (e.g., I decided to move closer to family after years of hemming and hawing over it), but I didn't feel relief from my depression symptoms right away. That happened about six weeks in: I started to feel that lighter feeling, and doing everyday tasks wasn't so hard.
Early on in the treatment, my guide, Shannan, an Aussie based in Tulum, Mexico (shoutout to Shannan — she's the best!), helped me process what I experienced during my treatments during online video chats called integration sessions.
One time, I went into a session with the intention/question: Why am I so depressed? I wound up seeing memories of family and didn't think they were relevant to my intention, but she helped me talk it out and make the connections that I had missed — kind of like a therapist does.
Once you get through the first round of treatment (six sessions) at Mindbloom, then it's a little more DIY and there are fewer integration sessions, unless you want to buy them. The idea is that you get the hang of it in your first six sessions and can purchase additional support if needed.
Who is a good candidate for ketamine treatment?
Dr. Yermus says that anyone dealing with depression or anxiety who is in good physical health and has an open mind is a candidate for treatment.
However, the government is a bit more exacting when it comes to prescribing the esketamine nasal spray. The FDA has only provided approval for the treatment of treatment-resistant major depression (meaning depressive episodes associated with major depressive disorder that have not responded to standard forms of oral antidepressants) and major depressive episodes associated with serious suicidal ideation and/or behavior, says Dr. Sanacora.
What does ketamine therapy cost, on average?
Unless you're taking esketamine, which is FDA approved and thus eligible for insurance coverage, you'll be paying about $450 for one IV infusion, on average, per WebMD . At Field Trip Health, one IM injection costs $750, and Mindbloom charges $89 a week for three months ($1,060) for new patients, which includes six ketamine treatments. Returning clients pay $59 per week for three months.
Note that all these companies offer support services before and after treatment, the cost of which is typically included in the aforementioned prices.
What are the risks of taking ketamine?
Dr. Sanacora points out that the long-term effects of taking ketamine for depression remain unknown. During research involving animals, ketamine was shown to cause some toxic effects on the brain as well as behavioral and cardiovascular side effects, he said . While some human studies have also shown evidence of behavioral and brain abnormalities linked to ketamine use, this has generally been in people who use the drug recreationally, he notes.
Also, ketamine — known by its street names Special K, Vitamin K, Kit-Kat, and Super K — has been used recreationally for decades, particularly in the 1980s. So there's a possibility for addiction if dosing isn't professionally monitored. As its Schedule III label indicates, ketamine has "a moderate to low potential for physical and psychological dependence," per the DEA .
Personally, I don't feel that I developed any kind of dependence on the ketamine, but I do feel drawn to the healing nature of the ketamine experience. My Mindbloom guide said that, after doing an initial round of, say, three months of treatments, many clients do a refresher course once a year afterward to keep reaping the benefits of therapy.
That's likely what I intend to do, and I can only hope that — for myself and others — ketamine treatment becomes more widely accessible and affordable in the future.
Related Articles
‘I Started Doing At-Home Guided Ketamine Treatments To Help With My Depression During Quarantine’
“Before I started using ketamine, I felt like I had run up against a wall in therapy.”

So how does ketamine work? For one, its been shown to boost the function of brain circuits damaged by stress, then later actually repair those circuits, per a study on mice in the journal Science . It can also up the number of serotonin receptors in the brain, found a small Swedish study , making it easier to absorb the “happy” hormone. For 72 percent of the 30 participants, this boost occurred within 24 to 72 hours, which explains why ketamine can provide rapid relief for depression.
For the 10 to 30 percent of people with depression and PTSD who don’t respond well to traditional drugs or treatments (mostly women, btw!), options like ketamine offer a new solution. Here, Melanie Lowery shares how ketamine helped her mental health amidst the coronavirus pandemic, and what it's like to do guided ketamine treatments at home.

I’ve struggled with depression and anxiety for most of my life and been on some form of SSRI since 1992. Those drugs worked for me, but only for a while . About 10 years ago, I started to feel like they were only “leveling off” my emotions, and then that baseline would gradually sink until I tried a new drug and the process started all over again.
At one point, I tried eight different kinds of drugs in one year, and the side effects were horrible: extreme fatigue, weight gain , no sex drive . I reached a point where I just didn’t want to feel numb anymore, so I started looking into alternative treatments.
It didn’t take me long to fall down the psychedelic rabbit hole in my research.
After a lot of Googling, I applied for clinical trials studying psilocybin (found in magic mushrooms) and MDMA , but I didn’t get in to any of them. I discovered there was legal psilocybin treatment in Jamaica and planned to drop a lot of money to travel there and try it. But in early March, right before the trip, a poster in New York City (where I was on sabbatical at the time) caught my eye. It read: “Psychedelic medicine is here.”
The poster was advertising a new ketamine treatment facility called Mindbloom , a mental health clinic run by licensed pros in psychiatric ketamine therapy, clinical psychology, and psychedelic research. I’d looked into ketamine IV treatment , which was really expensive, but this clinic offered a similar treatment with sublingual pills for as little as $150 per dose. I put the Jamaica trip on hold and went to the clinic instead.
After an initial evaluation to determine if I was a good candidate for this kind of treatment, I had my first session at their clinic in NoMad, New York City (which has since shut down due to COVID-19). The in-person sessions took place in a comfy, living room-like setting. I sat in a zero-gravity chair, the lights were low, and I wore a soft eye shade and headphones that pumped out a calming playlist. A psychiatric nurse practitioner stays in the treatment area the whole time. She gave me the pills, which dissolve in your mouth over a few minutes.

My first ketamine trip was a totally out-of-body, dissociative experience.
I didn’t see the Kool-Aid colors you always associate with psychedelics, but there were pleasant, low-level visuals. I know it sounds weird, but at one point, it felt like I dissolved into my atoms and they floated up into deep space to commingle with the stars. When I came out of it the very first time I was just ecstatic.
.css-1eiql25{text-align:center;margin:0rem;padding-top:0.9375rem;padding-bottom:0.9375rem;} .css-1cugboc{margin:0rem;font-size:2.125rem;line-height:1.2;font-family:Domaine,Domaine-roboto,Domaine-local,Georgia,Times,Serif;color:#f7623b;font-weight:bold;}.css-1cugboc em,.css-1cugboc i{font-style:italic;font-family:inherit;}.css-1cugboc b,.css-1cugboc strong{font-family:inherit;font-weight:bold;} “Before I started using ketamine, I felt like I had run up against a wall in therapy.”
I wasn’t cured of depression or anything, but it was such a vacation from myself that I was overwhelming grateful. Even if nothing happened long-term, having an escape outside of my body, outside of my cares, left me feeling so light. I walked home and slept for the rest of the day and most of the next, but then I was back to functioning normally. I knew I wanted to keep going in for treatments.

I was scheduled for one session a week, and then the pandemic happened.
Luckily, Mindbloom was already equipped for telemedicine sessions , so it was a smooth transition to at-home treatment. They sent me everything I needed to keep going on my own: a blood pressure cuff, an eye shade, playlists, anti-nausea medication, and the ketamine pills.
Before my sessions, I did a video consult with the nurse practitioner, and then my partner acted as my “trip-sitter,” occasionally checking in on me and touching my toes after an hour to make sure I was slowly coming back into my body again. Once the ketamine wore off, I debriefed again with the nurse practitioner over video call.
After my second session in mid-March, I noticed that I was doing more around the house; I wasn’t over-sleeping. I was just able to function better. I was feeling good, especially given the stress of the pandemic .
After the third at-home treatment at the end of March, I noticed a real lift in my mood. I went outside and actually said, “Oh, it’s so pretty today.” I noticed I could smile without it being fake. After three home sessions, my partner and I moved to Florida for a few months, where I was able to continue treatment. Now, I’ve completed three rounds, with four sessions each, and recently started on a fourth round of treatment.
Before I started using ketamine, I felt like I had run up against a wall in therapy . Now I feel better than ever.
There was nothing else to talk about anymore in traditional talk therapy for me, without my ketamine experience to complement it. But with the help of this medicine, I’ve dredged up so much stuff to unpack and discuss with my therapist. I increased my talk sessions to twice a week because I had so much to get through.
“It was such a vacation from myself that I was overwhelming grateful.”
I feel like my brain is changing too. I no longer want to drink—I don't like the numbing quality anymore. I make more connections and associations between things around me, like something I see or a song, and a memory, and that integration between my outer world and inner world feels so meaningful.
Honestly, I feel like I’m 100 percent in remission from depression . I’ve spent almost my whole life on pharmaceutical drugs, and I'm so glad that's over, at least for now. (I weaned off of my SSRIs safely, with my clinician in the know.) I can do these ketamine sessions every few weeks and go about my normal life in between without all the awful side effects I had before. The negative was outweighing the positive when it came to the pharmaceutical drugs I was taking. I feel like I've finally found a sustainable solution.

Eventually, I may not need ketamine to maintain my mood, but I don’t want to stop treatment.
It’s enjoyable for me and I only want to go deeper with my introspection. I feel like ketamine is preparing me for when psilocybin is legal, and then I’ll be able to do even further self-exploration through that. My friends think the treatment sounds a little weird—I get a lot of “But isn’t that a horse tranquilizer?” or, “Wait, is that what ‘Special K’ is?” I try to explain that yes, it’s the same thing, but the way it’s used—in a safe, controlled environment, in combination with therapy , is completely different.
No one can really argue with the huge shift in my mood. They’re happy, and a little bit blown away, with how much better I’m doing.
This article appears in the October 2020 issue of Women’s Health. Subscribe now .

Mental Health

How To Tell If You Have ‘Popcorn Brain’ Or ADHD

How Your Teen BFF Could Affect Your Future Health

Why Simone Biles Called Aly Raisman 'Grandma'

Orthorexia, A Form Of Disordered Eating, Is Rising

How Therapy Helped Jade Carey Make Olympic Team

Simone Biles Had Therapy The Day Of Gold Medal Win

The 4 Best Ice Bath Tubs For Recovery

Taryn Kloth and Kristen Nuss Pregame Ritual

Laurie Hernandez On Mental Health Post-Retirement

Suni Lee Visualizes Gymnastics Routines Before Bed

How To Try The 'Cognitive Shuffling' Sleep Hack
Find anything you save across the site in your account
Ketamine Therapy Is Going Mainstream. Are We Ready?

In the fall of 1972, a psychiatrist named Salvador Roquet travelled from his home in Mexico City to the Maryland Psychiatric Research Center, an institution largely funded by the United States government, to give a presentation on an ongoing experiment. For several years, Roquet had been running a series of group-therapy sessions: over the course of eight or nine hours, his staff would administer psilocybin mushrooms, morning-glory seeds, peyote cacti, and the herb datura to small groups of patients. He would then orchestrate what he called a “sensory overload show,” with lights, sounds, and images from violent or erotic movies. The idea was to push the patients through an extreme experience to a psycho-spiritual rebirth. One of the participants, an American psychology professor, described the session as a “descent into hell.” But Roquet wanted to give his patients smooth landings, and so, eventually, he added a common hospital anesthetic called ketamine hydrochloride. He found that, given as the other drugs were wearing off, it alleviated the anxiety brought on by these punishing ordeals.
Clinicians at the Maryland Psychiatric Research Center had been studying LSD and other psychedelics since the early nineteen-fifties, beginning at a related institution, the Spring Grove Hospital Center. But ketamine was new: it was first synthesized in 1962, by a researcher named Calvin Stevens, who did consulting work for the pharmaceutical company Parke-Davis. (Stevens had been looking for a less volatile alternative to phencyclidine, better known as PCP.) Two years later, a doctor named Edward Domino conducted the first human trials of ketamine, with men incarcerated at Jackson State Prison, in Michigan, serving as his subjects. At higher doses, Domino noticed, ketamine knocked people out, but at lower ones it produced odd psychoactive effects on otherwise lucid patients. Parke-Davis wanted to avoid characterizing the drug as psychedelic, and Domino’s wife suggested the term “dissociative anesthetic” to describe the way it seemed to separate the mind from the body even as the mind retained consciousness. The F.D.A. approved ketamine as an anesthetic in 1970, and Parke-Davis began marketing it under the brand name Ketalar. It was widely used by the U.S. military during the Vietnam War, and remains a standard anesthetic in emergency rooms around the world.
Roquet found other uses for it. After his lecture in Maryland, he offered experiential training to the clinicians there. “I was introduced to the strangest psychoactive substance I have ever experienced in the 50 years of my consciousness research,” the psychiatrist Stanislav Grof recalls in “ The Ketamine Papers ,” a book edited by the psychiatrist Phil Wolfson and the researcher Glenn Hartelius. Grof subsequently experimented with ketamine personally, and found himself inhabiting the perspectives of a wet towel hanging on a railing overlooking the ocean, petroleum filling the cavities of the earth, and the prisms of a diamond. “In one of my ketamine sessions, I became a tadpole undergoing a metamorphosis into a frog, and in another one, a giant silverback gorilla claiming his territory,” Grof writes.
When the training took place, psychedelic research was already coming under legal threat. In 1968, the U.S. government outlawed possession of LSD; Richard Nixon announced a war on drugs three years later. In 1974, Roquet was jailed for several months in Mexico, and subsequently cut back on his group sessions. (He died in 1995.) The Maryland Psychiatric Research Center ended its psychedelic research in the mid-seventies, amid broader upheaval at the center.
But ketamine remained medically legal, and countercultural psychiatrists continued to experiment with it. In the eighties, the drug’s best-known enthusiast was John C. Lilly, a doctor and psychoanalyst perhaps most famous for using sensory-deprivation tanks and dabbling in human-dolphin communication. Lilly became addicted to ketamine: a researcher who crossed paths with him at the Esalen Institute, a retreat in Northern California, recalled Lilly spending most of his time in his Volkswagen minibus, where he was evidently injecting himself multiple times a day. (Lilly said that he stopped using the drug in his early sixties, on the orders of extraterrestrials, but he resumed taking it later in life. He died in 2001, at eighty-six.) During these years, ketamine also became a popular dance-floor drug. Partyers generally snorted it, at lower doses, for a less drastic and more interactive high, experiencing distortions of perception that have been described as “scenery slicing” and “environmental cubism.” Among clubgoers, taking so much that you became unaware of your surroundings—experiencing a “K-hole”—was typically considered a scary mistake. The drug became especially fashionable among ravers in the nineties, and, at the end of that decade, the U.S. government made ketamine a Schedule III substance, putting it on the same regulatory footing as steroids and Tylenol with codeine.
Meanwhile, clinicians at Yale, who were using the drug to mimic the symptoms of schizophrenia, noticed that ketamine improved people’s moods. Researchers began studying it as a treatment for depression, and, in 2006, the National Institute of Mental Health concluded that a single intravenous dose of ketamine had rapid antidepressant effects. Around three hundred clinical trials have since been held; the broad consensus is that ketamine relieves symptoms of depression for a period that can last days or weeks, during which time talk therapy often proves more effective than normal. Ketamine is what’s called a “dirty drug,” meaning that it acts on different parts of the brain at once, and there are several theories about how it works against depression, but most focus on its effects on certain receptors in the brain, and on the neurotransmitter glutamate. (One theory holds that ketamine modulates levels of a protein that can generate new neurons.) By 2010, doctors were recommending its off-label use to acutely suicidal patients, and ketamine clinics began opening around the country. These days, the research and debate surrounding ketamine are less concerned with whether it can treat depression than with how it works, which delivery method makes it most effective, and how drug companies and health-care providers might best profit off a substance whose patent expired in the nineteen-eighties.
One of the first clinics, New York Ketamine Infusions, was opened by Glen Brooks, a Harvard-trained anesthesiologist, in 2012. Brooks sometimes wears a white lab coat, and practices in an ordinary-looking doctor’s office, where he keeps jars of FireBall candies on his desk. (He used to sublet space from a podiatrist.) He’d been a physician for more than thirty years when a relative’s drug problems prompted him to pursue addiction medicine. After just a few months, he concluded that the field was hopeless when it came to addressing the childhood traumas that lead people to self-medicate. He read the early research on ketamine as a treatment for mood disorders and saw not only reason for optimism but a business opportunity.
Brooks administers ketamine by I.V., at subanesthetic doses, and only some of his patients have dissociative experiences. “There’s nothing therapeutic going on when they’re here,” he told me, when I visited him at his clinic on a rainy Sunday this past spring. Patients hooked up to I.V. drips were undergoing treatment in dimly lit rooms. “We’re growing dendrites and synapses,” he said. Brooks encourages his patients to bring a friend or listen to a podcast to distract themselves from ketamine’s psychoactive effects. He said that what patients happen to think about during their sessions doesn’t really matter.
This approach, which is typical of the early ketamine clinics, contrasts with the countercultural attitude that prevailed among the drug’s advocates in the seventies and in a new tide of startups. Beginning roughly with the publication of “ How to Change Your Mind ,” a best-selling book by Michael Pollan, in 2018, psychedelic treatments for mental health have gone mainstream. Publicly traded companies, such as Compass Pathways and MindMed, have begun patenting variations on psychedelic treatments. Last fall, Peter Thiel was among the investors in a hundred-and-twenty-five-million-dollar round of funding for the biotech company atai Life Sciences, which principally focusses on the use of psychedelics in the treatment of mental illness; in June, the company went public, and was valued at more than three billion dollars.
In recent years, I have watched many people in my life quit antidepressants and start microdosing LSD and mushrooms, informed by exuberant news reports and the encouraging but not yet conclusive data documented in Pollan’s book and elsewhere. Most of these people are skeptical of the pharmaceutical industry and desperate to find more pleasure in life; for some, coding substance use as an antidepressant routine, and ingesting very tiny doses, seems to suit a sense of middle-class propriety and upwardly mobile productivity. (The doctors I spoke with by and large agreed that ketamine—which a number of outlets have proclaimed the “It Drug” of personal use during the pandemic—does not have the same clinically proven antidepressant effects when snorted.)
It is also, unlike LSD and mushrooms, legal for medical use throughout the U.S., and so provides the only avenue for American medical providers to generate revenue with psychedelic substances. (In 2019, the F.D.A. approved Spravato, from Johnson & Johnson, which contains one of the two molecules in the original ketamine formulation, and which will allow the company to sell a more profitable, if not necessarily more effective, version of the drug.) Today, a self-referring depressive with several hundred dollars on hand who is not in the throes of active mania or psychosis can seek out a wide array of clinical treatments with the drug: a titrated dose given intravenously by an anesthesiologist at a retail clinic, a shot in the arm from a psychiatrist in private practice, an oral lozenge sent in the mail by a startup taking advantage of pandemic-era changes to the regulation of remote prescriptions. If you can get to the right city, and have sufficient funds, you can easily secure a legal, therapist-guided, mind-expanding trip at a clinic that advertises on Facebook and is funded by venture capital.
The New York office of Field Trip Health, which opened in August, 2020, is situated in the Kips Bay neighborhood of Manhattan. It occupies the entire eleventh floor of a building next to Baruch College, and has big windows and a wraparound terrace. The decorative touches are spa-like: white rugs, fiddle-leaf figs, electric candles inside glass-paned lanterns. The aesthetic seems based on the assumption that, when a company hopes to take a formerly taboo practice mainstream, a West Elm interior can go a long way.
When I visited, this past spring, Matt Emmer, Field Trip’s vice president of health-care practice, showed me around—he was wearing a floral button-down of the sort that I associate with tech-company business casual. Field Trip was founded, in April, 2019, by five Canadian entrepreneurs, four of whom previously founded a chain of cannabis-dispensing medical clinics. The company now operates ten ketamine clinics in Canada and the U.S., with plans to open several more in the near future. (Field Trip recently opened a clinic in Amsterdam that offers patients guided-therapy sessions with magic mushrooms.) The company has a research and development wing, Field Trip Discovery, which is devoted to the cultivation of psilocybin mushrooms and the development of psychedelic-inspired medicines; this work is being done at a laboratory at the University of the West Indies, in Mona, Jamaica, where the drug laws are relatively forgiving. Field Trip recently filed a patent for a molecule called FT-104, which, according to preclinical experiments, targets the same serotonin receptor as psilocybin, but has much briefer effects. A drug trip that lasts two hours offers a far more viable business model than one that lasts five or six.
Emmer walked me down a hallway where the sound of water burbled from a white-noise machine, and he told me that he took interior-design cues from nature (“something that’s universal”). In the reception area, I saw copies of “How to Change Your Mind” for sale alongside “ Be Here Now ,” by the psychedelic guru Ram Dass. But, for the most part, signs of the counterculture were muted. Emmer led me into a windowless room. On one wall was a mural of spider monkeys peeking through palm fronds. In a corner, there was a large, white leather, zero-gravity chair. I sat down, and, at Emmer’s invitation, pressed a button on a remote. The chair made a soothing hum and slowly tipped backward, ready to carry me across the threshold of consciousness in its arms. “It makes you feel as weightless as possible without going into space,” Emmer said. This was one of the treatment rooms.
Sitting where the therapist normally would, Emmer explained the process. A patient arrives and selects from a menu of guided meditations and light therapy as a way of easing in before her trip. Ketamine is then administered with one or two intramuscular shots—the mind-altering equivalent of a rocket launch. The patient puts on noise-cancelling headphones, a weighted blanket, and an eye mask, and turns inward, listening to a soundtrack of nonverbal music. (One playlist is mostly classical and another is electronic; the music is intentionally obscure, to avoid provoking personal associations.)
I pressed another button on the remote, and Emmer waited as my chair slowly returned to its upright position. After the ketamine subsides, he explained, the patient sits for a session of talk therapy. The entire round of treatment lasts between two and three hours. A lounge stocked with mandala coloring books and watercolors offers a restful place to come back to earth before going home. Like most ketamine clinics, Field Trip encourages an initial set of four to six infusions spaced out across two to four weeks, with boosters available on an as-needed basis thereafter. The first session costs seven hundred and fifty dollars and subsequent treatments cost a thousand. The patient is paying for the therapy more than the drug, which costs as little as seven dollars a dose.
Earlier this year, a thirty-five-year-old filmmaker I know signed up for ketamine-assisted therapy at Field Trip. She had been reading about psychedelics during the pandemic. She read the Pollan book and a memoir called “ The Wild Kindness: A Psilocybin Odyssey. ” She listened to a lot of podcasts. She had tried LSD and mushrooms before. On those trips, she felt expansive and connected to the cosmos; she looked at the clouds, which seemed to be moving backward, and at the moon, which appeared more three-dimensional than usual. She wanted to undergo other shifts in her perspective. She was experiencing a degree of anxiety and obsessive thinking—she takes antidepressants and has more than a decade of therapy in her past—but she did not believe that she had any urgent mental-health issues. “I’m actually in a good place in my life right now,” she told me, “and it’s more about wanting to take it to the next level.” She contacted an underground therapist about a supervised mushroom trip, but the waitlist was two years long. “This was the path of least resistance,” she explained to me, of Field Trip. “I literally typed something into Google.” She underwent two screenings with the clinic, the first of which focussed on what ketamine is and what it can offer, and the second of which, she told me, was “about making sure you’re not crazy or you’re not going to kill yourself afterward.”
Her first session was scheduled for June. I spoke to her later that week. The experience had been more intense than what she was expecting. Her intake sessions were conducted virtually, so the day of her trip was her first visit to the office. An employee showed her a chair with a kind of helmet that descends upon the sitter’s head and provides a choice of colored lights to set the mood for meditation. She saw a glass table with a tray underneath it, in which a self-propelled metal ball traced patterns in sand. “I felt like I was already tripping when I went in there,” she told me. She found the burbling water sounds from the white-noise machine unnerving.
They put her in a room with a jungle-themed mural at the end of a long hall. She lay down in the anti-gravity chair and waited for its slow, dental-office recline. A nurse took her blood pressure and then presented a syringe of ketamine in a bronze Tibetan bowl. “I had to stop myself from cracking up,” she said, “because I didn’t want to be laughing at them, but there was something about it that was so absurd.” After the shot, she put on her eye mask and waited. She thought of her poodle at home and told the therapist that she was worried about her, but she calmed down after remembering that her partner was coming home early from work that day and would take care of the dog. She was given a second shot, and images began rushing through her mind: indecipherable hieroglyphics, ancient calligraphy. She saw herself onstage at a Q. & A. for one of her films. She experienced a kind of consciousness without identity. She felt as if she were inside a cardboard box with only a small hole of light and she was tearing at the aperture to widen it. She lifted her eye mask and looked down at her hands, and thought, Oh, wow, I’m a human. But she couldn’t remember where or who she was. Then she was overwhelmed with nausea, which happens to a modest subset of people who inject ketamine. She cancelled her second session immediately afterward. “I still feel so out of sorts,” she told me.
But, a few weeks later, she was ready to return. At her second session, she received a lower dose, and the effects of the drug were milder. She saw a sea of waving Japanese maneki-neko cat figurines and tried to find her mother’s face among them. A day or two later, she began to have a recurring feeling that seemed new. “This new feeling was, What if it works out?” she told me. It was a hopeful, expansive feeling. Then, one day, it was gone. “I guess it’s worn off or something?” she said. “It’s funny how it’s something you can’t talk yourself into feeling.”
For the countercultural therapists who have been administering ketamine to their patients for years, the current boom is seen with bemusement and not a small amount of worry. Phil Wolfson, who co-edited “The Ketamine Papers,” first took ketamine in 1990, and began giving it to select patients twenty years later. (Prior to that, he had used MDMA in therapy, but stopped when the drug became a Schedule I substance, in 1985.) Now in his seventies, he has trained many psychotherapists in the use of ketamine, including several at Field Trip Health. In his own practice, he offers both psychotherapy with lozenges and more intense guided trips with intramuscular injections. He is fluent in the neuroscientific theories about how ketamine works but regards them as reductionist. “Everything causes neuroplasticity,” he told me. “Having great love, or climbing a mountain, or having a terrible tragedy—it all creates movement of dendrites”—the branched tips where neurons form pathways—“because movement of dendrites is an essential adaptive function. We change because of experience.” We were speaking on the day after the anniversary of Wolfson’s son’s death, more than thirty years ago, from leukemia, at the age of sixteen, which Wolfson honors each year with a memorial.
Wolfson, who has a corona of silver hair and whose New York accent has resisted decades of living in California, is not eager to categorize ketamine as an antidepressant. Change is not merely a chemical by-product, he told me, and diagnostic categories help only up to a point. He believes that ketamine’s particular power is in the way that it offers a “subjective time-out.” Unlike ayahuasca or mushrooms, which often produce visions that coalesce into narratives, ketamine usually gives a brief experience of the void. “Ketamine really makes no sense,” he said. “It’s not attached to subjective experiences—themes don’t occur, or, if they do, they might not be particularly psychological in nature. I’m not reformed by neuroplasticity; I’m reformed by having had a break from the obsessions of my mind.”
The most striking results from ketamine therapy do not involve people like my filmmaker friend, who has manageable anxiety, but those who are experiencing chronic, treatment-resistant depression. Zachary Rice, a twenty-eight-year-old TV writer, has seen a therapist since he was ten. At sixteen, he was diagnosed with clinical depression, and in his early twenties he was diagnosed with acute post-traumatic stress disorder and obsessive-compulsive disorder. He began taking antidepressants at eighteen; since then, he has been prescribed thirteen different medications and has attempted suicide. In March, 2020, as the pandemic started to spread, he became suicidal again. He spoke with his therapist and psychiatrist on the phone. Concerned that more medication wouldn’t help him quickly enough, they gave him two options: hospitalization or ketamine. “I basically only knew it as a gay party drug or a horse tranquilizer,” he said.
That call was on a Friday. The following Monday, Rice went to a clinic in Brooklyn Heights called Ember Health. Ember was started by an emergency-medicine physician named Nico Grundmann and his wife, Tiffany Franke, a strategy consultant, in 2018. Ember makes no reference to psychedelic experiences in its marketing materials, and, in conversation, Grundmann seemed wary of the term “psychedelic,” saying that it could scare some patients away. But the altered state of mind produced by ketamine is a fundamental aspect of the company’s approach to treatment, he said. The company’s office has rugs and sofas and herbal teas—“like a well-appointed home,” he told me. He said that Ember tries to take the most evidence-based approach, which is to administer ketamine by I.V. infusion, not intramuscular injection, at a dose of 0.5 to one milligram per kilogram of a patient’s weight. Ember does not offer psychotherapy in-house, but the company only accepts clients who are actively being treated by mental-health professionals.
Rice had never taken psychedelic drugs before—he’d always worried about how they would interact with his medications. On the intake questionnaire, he got a perfect score: severe depression. He recalls thinking, “If this doesn’t work, at least I get to try a cool drug and I know I won’t die, because I’m in a doctor’s office.”
Rice put on an eye mask and a pair of headphones and was hooked to an I.V. drip and a cardiac monitor. He was encouraged to think about a happy moment, so he thought of standing on the outer rim of Yosemite Valley and watching the sunset with his friends. “Then it was as if the lights dimmed in a movie theatre and reality went away,” he recalled. “I flew across the valley at five thousand miles an hour and smashed into Half Dome, then Half Dome exploded into the universe and I was floating in space.” A narrator coalesced, a kind of entity or guide, with a commanding yet comforting voice. (He sounded like Danny Glover, Rice said.) He asked Rice if he wanted to take a tour of his own brain. Rice proceeded to greet all the people who work in his brain, and then the tour moved on to the formative experiences in his life, including deeply traumatic ones that he considers the roots of his mental illness. He saw a mosaic of every person who loves him and has been important to him. “You don’t have to scare them anymore,” the narrator said. “You can be alive and it’s O.K. and it’s good.” It was the first time in twenty years, Rice said, that he’d had anything like a positive internal monologue. The tour concluded with an “interdimensional safari” where he watched elephants twirl until the safari car folded back onto itself and his brain merged with the driver’s. When Rice regained normal consciousness, he was laughing and crying.
He was given tea and wrote down what he’d seen. Then he took the elevator back down to the streets of Brooklyn. Outside, everyone was wearing masks, and a pigeon pooped on him. He walked into a park and looked at the birds, crying at their beauty. He went home and did chores he had put off for years. “It was literally like entering life for the first time,” he told me, comparing it to the process of color correction when making a film. “Ketamine color-corrected for my existence. I saw the world as it was, without this heavy gray mass.”
Rice did four sessions across ten days, and he has done monthly sessions ever since. Each session is distinct: sometimes, he gets no visions at all, and sometimes he feels like he is in a Windows 95 screensaver. “I’ve died in ketamine sessions,” he said. “I’ve met what I was meant to understand was God.” The sessions are five hundred dollars each, but sixty per cent of the cost is covered by his insurance. He can tell that the effect of a session is wearing off when daily tasks start to feel insurmountable, he said. “It’s not hyperbolic to say that ketamine saved my life,” he said. “That hour session was more transformative for my mental health than anything I’ve done in my twenty-plus years of therapy and medication.”
Field Trip, in contrast to Ember Health and New York Ketamine Infusions, seems to be interested in a broader customer base than those who are treatment-resistant. Ben Medrano, the New York clinic’s medical director, told me that he first tried ketamine and other psychedelic drugs as a raver in the nineteen-nineties, and that the spiritual benefits of such experiences should be extended to people who are uncomfortable sourcing drugs illicitly but could use a break from their ordinary mind. These benefits will never be easily verifiable in a laboratory or a double-blind study, he told me. “These are healing tools that access the potential of consciousness,” he said. “And, at the end of the day, we, as scientists, can’t talk about that much, because what do we say? We don’t even know where consciousness resides.”
If going to the doctor for a guided trip becomes as routine, for some, as getting Botox, there will surely be a bifurcated clinical scene: one for people who like hippie stuff and one for people who want nothing to do with it. In late June, I drove to the Catskills to watch a group of people receive training in ketamine-assisted psychotherapy at the Menla Institute, a Buddhist retreat center. There were a number of psychotherapists, but the group also included an E.R. physician, a military veteran who works to bring psychedelic-assisted therapy to fellow-veterans who have P.T.S.D., and an executive with a Miami-based startup called Nue Life.
Also in attendance was the psychiatrist Bessel van der Kolk, whose book “ The Body Keeps the Score ,” first published in 2014, frequently ranks among the ten best-selling books on Amazon. Van der Kolk told me about his experience working on the first studies of Prozac and Zoloft as treatments for P.T.S.D. “They weren’t bad,” he said, but they didn’t cure anyone, he noted, adding, “All you get now is drugs that by and large don’t work.” Van der Kolk had received an injection of ketamine from Wolfson a few years before. “I was blown into the universe,” he told me. “I had no mental experience—I lost my body, I lost my mind.” He emerged from his trip skeptical that ketamine could do anything, but his wife and collaborator, Licia Sky, noticed changes in him afterward. “Before, there was like this undercurrent of impatience, like this readiness to be agitated,” Sky, who was also at the training, told me. “That agitation got very quiet, but your power stayed,” she went on, turning to her husband. “That doesn’t mean that we don’t disagree about things. It means that there’s a level of urgency that’s gone.”
It was an exquisite day in Ulster County. The sky was a bright blue and the mountains were a lush and vivid green. The trainees gathered in a large, wood-beamed room, at the front of which stood a shimmering gong, flanked by a trio of Tibetan wall hangings. Wolfson had set up a small altar to one side, with a framed photograph of his son. It was the fourth day of the training. Half the workshop’s participants would be receiving injections, and the other half would watch over them. On the walls, large pieces of paper bore descriptions of the previous day’s trips. Among the phrases people had written down were “breath of God” and “saw ancestral stuff.” In a corner of the room, a woman prepared for her journey with some yoga asanas. Others filtered in from a vegetarian breakfast in the retreat center’s dining hall and settled onto mats and pillows laid out on the floor.
The session began with an invocation and the recitation of a poem by Rumi. An assistant brought out paper coffee cups labelled with the participants’ names: each contained a syringe with a dose of ketamine. For the next hour, I watched the therapists undergo their training. The trip sitters monitored them closely, occasionally taking notes or mirroring their movements. A sort of drumming-and-didgeridoo song played over speakers, followed by a track that prominently featured a rainstick. The woman who had been doing yoga flung her arms out wide and moved her body ecstatically. Toward the back of the room, a man began to sob, and an assistant came to Wolfson for advice. “We need to help him listen to the music,” Wolfson whispered.
After an hour, the group began to emerge from their trips. Wolfson took the microphone. “Relax into your being,” he said. “Find great peace, find your heart for yourself, find great compassion.” Assistants circulated with a tray of orange slices and the group began sharing what they had experienced. It was “not so much a seeing journey as a feeling journey,” one said. Another said that his experience in a prior session, with a lower dosage of orally ingested ketamine, had felt more beneficial—on the higher, intramuscular dose, he had gone to “fractal land, to the matrix, and being that far out you don’t do the work,” he said. A third person said, “Our inner children who are bereft long to be safe with their tears.” Van der Kolk, who had taken a moderate dose, of sixty milligrams, had been enamored with the soundtrack. “Every sound becomes a vision, every sound becomes a shape,” he said. Someone else said, “Well, what this weekend has done has given me a real appreciation of trance music.” The trainees then had lunch and attended a seminar about attachment theory.
I like hippie stuff, so when I decided to take a guided ketamine trip, I did so with Wolfson. Prior to my appointment, I completed questionnaires that evaluated my family history and whether I had experienced violence, trauma, or depression. In mid-June, I went to the lower Manhattan office of Gita Vaid, a psychiatrist and psychoanalyst in private practice who had also been at the training in the Catskills. There, Wolfson, Vaid, and I talked for an hour. I told them that I was struggling to recover from a bad experience the year before. I had taken some time off work, gone to therapy, and gone back on antidepressants for the first time in almost a decade, but I seemed unable to regain stability, or the sense of belonging that had once held me in the world. Then, Wolfson, drawing on our conversation, recited a personalized invocation to send me on my way. I lay down on a couch and Vaid put an injection in my arm.
My mind dissolved into a muted silence, as though I were in a warm, carpeted soundbooth. I had taken an initial dose of thirty-five milligrams, and no specific visions coalesced, but the soundbooth walls began to collapse, like the C.G.I. sand in “The Mummy,” and swirled into shifting shapes, blown around by gusts of a mysterious wind. It was like being immersed in a world of iron filings, drawn into patterns by a magnet in a dimly lit forge. Twelve minutes after the first shot, I was asked if I wanted the second injection, also of thirty-five milligrams. The question seemed to come from very far away, and I was surprised that I could articulate a response. Vaid lifted my sleeve and gave me another shot. Now, I was in a velvet painting; I was sinking into the carpet; I was under the canopy of a primeval forest, on its mossy floor, hidden under ferns. I wanted to sink deeper into the primordial nothing, but, in time, I became aware of my body again. Before taking the shot, I had been sad and worried. I emerged feeling calm and soothed. As psychoactive experiences go, it was five stars, truly enjoyable. All I could repeat, stupidly, as I regained awareness of my surroundings, was how “cool” it had been.
I’d done ketamine at parties before, and liked how it fragmented sensory input and seemed to dilate time; the experience of injecting it was far more intense. It was as if I had taken a different drug altogether. During the previous year, I had become increasingly skeptical of the enthusiasm for psychedelic drugs as a revolution for mental health. This may have involved some mild hypocrisy, since I have done psychedelics and have found that, in addition to being fun, they sometimes helped me gain perspective and process difficult experiences. I was uneasy about pinning messianic potential on any particular mind-altering thing, and I felt aware of the limits of what such substances could do. I also feared the warping effects of the profit motive. As I researched this article, I began getting Facebook ads for a controversial company called Mindbloom, which sends ketamine lozenges in the mail to be taken between scheduled video sessions with a trained guide. The ads include a quote from someone saying, of ketamine treatment, “Before I started, I felt like I had run up against a wall in therapy.”
Wolfson, the first time we spoke, told me, “There’s this huge population of chronically depressed people in a chronically depressing world that’s making more chronic depression.” In other words, the way we live is making us sick. The suicide rate in the U.S. has increased by nearly thirty per cent since 1999; from April 2020 to April 2021, a hundred thousand Americans have died of drug overdoses, many of them presumably medicating themselves out of the difficulties of ordinary consciousness. In “The Ketamine Papers,” Wolfson offers “a very partial list of antidepressants.” On his list: “anticonvulsants, stimulants, marijuana, exercise, meditation, hedonism, temporary satisfaction of cravings, elimination of cravings, oxytocin, sexuality, spiritual practice, money, love, children, activism, justice, a good job, respect, friendship, education, a good book, a bad book, and so on.”
Ketamine is generally considered safe when used at sufficient intervals, but, when snorted or injected daily for long periods of time, it can cause increased tolerance, cravings, withdrawal, and permanent urinary-tract and kidney damage. It may also affect long- and short-term memory. “You do see these sort of unique personalities that are inclined to it,” Ben Medrano, of Field Trip Health, told me, of the risks of ketamine addiction. “Like, John C. Lilly was an astrophysicist who studied dolphins.” But Medrano was insistent that it’s only “a subset of people who are prone to it.” The government classifies ketamine’s abuse potential as moderate to low. Still, the risk of overuse has long been acknowledged in underground circles. In “ The Essential Psychedelic Guide ,” published in 1994, the researcher D. M. Turner writes, “A fairly large percentage of those who try Ketamine will consume it non-stop until their supply is exhausted. I’ve seen this in friends I’ve known for many years who are regular psychedelic users and have never before had problems controlling their drug consumption.” Turner died in a bathtub on New Year’s Eve in 1996, apparently having drowned after injecting himself with ketamine.
Multiple doctors who conduct ketamine therapy assured me that they do not accept patients who are exhibiting drug-seeking behavior, and also told me that, at the pace of treatment practiced by responsible clinicians, there is minimal risk of dependency or of the urinary-tract infection known as ulcerative cystitis. But the pandemic had brought home to me some indelible lessons about the fragility of the mind. Wolfson was more willing than most of the physicians I met to acknowledge this fragility. “Anyone doing this work as a therapist will come across those folks who become too attached to a drug or drugs, who make broad mistakes, lose their relationships, even themselves,” he once wrote, in a consideration of Lilly, the ketamine user who lost his way. The best-known risk for people who dabble with psychedelic states is still, as Wolfson puts it, “the loss of the monitor that overrides and guides us through the labyrinth of life, as best as it can.”
Wolfson and Vaid told me that I could recover in the waiting room for as long as I needed, but I was impatient to return to the world. I stepped out onto the street into the late afternoon with a wobbliness familiar from years of leaving nightclubs after daybreak, my arms sore as if I had just gotten two COVID vaccines at once. The apartment buildings along University Place were vaguely changing sizes, so I walked across the street to a nail salon and used a pedicure as an excuse to sit in a chair for forty minutes and let my gaze go out of focus. By the time the polish was dry, I had returned to baseline. I had skipped lunch to avoid getting nauseated, so I found a place where I could eat dumplings. Then I met up with friends in the East Village, where the Friday-evening atmosphere in the streets had the uncorked chaos of a belated spring break.
The next day, I felt different. I did some things I had put off for a long time, and stopped obsessing over other things that had monopolized my thoughts for weeks or months. Perhaps I had been primed to feel this way by the research I had read, but my state of mind seemed only indirectly related to anything I’d seen on my ketamine trip, and entirely unrelated to any kind of therapy. It seemed physical in nature. My mind was working the way I often wish it did. I had, in the past, tried to achieve this state of mind through drinking caffeine, through not drinking caffeine, through exercise, sleep, meditation, antidepressants, healthy eating, Vitamin B 12 , magnesium, amphetamines, yoga. My mind had always seemed resistant to on-demand engineering. This new feeling was neither an afterglow nor a state of stimulation. It felt like stability. I didn’t want to drink alcohol, or even coffee, out of a fear that the feeling would abandon me; I dreaded being thrown back into my ordinary mind. The feeling lasted a little more than two weeks, and then it went away. The memory of what it had felt like lingered a bit longer, and then it went away, too.
New Yorker Favorites
An Oscar-winning filmmaker takes on the Church of Scientology .
Wendy Wasserstein on the baby who arrived too soon .
The young stowaways thrown overboard at sea .
As he rose in politics, Robert Moses discovered that decisions about New York City’s future would not be based on democracy .
The Muslim tamale king of the Old West .
Fiction by Jamaica Kincaid: “ Girl .”
Sign up for our daily newsletter to receive the best stories from The New Yorker .
Is tripping with a therapist the next big thing In mental health?
- Clinics like Mindbloom and Field Trip Health want to make "psychedelic medicine" mainstream.
- Mindbloom went virtual in 2020, offering at-home ketamine treatments. Field Trip's spas are open.
- Research has shown that ketamine can help reduce depressive symptoms, but experts urge caution.

Last fall, Dan, a 43-year-old father of 2, confided in a friend that he was buckling under the stresses of daily life in the midst of a global pandemic. When a friend told him about Mindbloom, a telehealth start-up offering an at-home ketamine treatment, he was intrigued.
A few days after that, a Mindbloom-branded journal, pen, and eye mask arrived in the mail. His medicine—oral ketamine tablets in a holographic package—arrived shortly after from Mindbloom's pharmacy partner.
"I wanted to be less reactive, to learn to trust myself," said Dan, who had struggled with a general anxiety disorder and ADHD for many years. (He asked that his full name not be used.)
When it came time for his first session, he sat down in his favorite chair, tucked the ketamine tablets into his cheek so they could dissolve, pulled his eye mask down, and waited. Later he would read back what he had written in his journal: "Whoa what an experience, me now versus me before is totally different."
An hour later, he was videochatting with his Mindbloom "guide," trying to process the experience.
Say hello to the next big thing in mental health.
Related stories
For years, momentum has been building toward a brave new world in which psychedelic drugs , such as psilocybin, MDMA, and even LSD become accepted and approved mental health treatments. Although major strides have been made—MDMA is in final-stage clinical trials now—to bring these drugs out of the rave and into the pharmacy, none of them are likely to be available for at least another few years.
Enter ketamine , which is best-known as the party drug, Special K, and has been available as an anesthetic since the 1970s. Ketamine has been used off-label as an antidepressant for the last decade in so-called "ketamine clinics," after researchers found that non-sedating doses of it led to relief from depression in the early 2000s.
Clinics like Mindbloom (tagline: "Psychedelic Medicine is Here") are trying to make ketamine more accessible by lowering the costs of the treatments, which aren't covered by insurance. Four sessions at Mindbloom will run you $1,000, compared to infusions done at a ketamine clinic, which can cost anywhere between $400 and $2,000 per session. Mindbloom serves clients in 11 states: New York, California, Florida, New Jersey, Pennsylvania, Nevada , Virginia, Arizona, Colorado, Texas, and Utah.
"Mental healthcare was the no. 1 public health crisis in America before COVID, and the pandemic's omnipresence in our daily lives has made the problem worse," says Dylan Beynon, Founder and CEO of Mindbloom. "Mindbloom is on a mission to transform lives to transform the world. We're doing this by radically increasing access to the next generation of mental health and wellbeing treatments."
But the real key to what these new upstarts are offering is the experience of the drug combined with integration coaching. (Most Mindbloom guides have some training in "psychedelic integration" from schools like the California Institute of Integral Studies. In addition to the post-treatment talk sessions, clients can text with their coaches.)
Field Trip Health is a similar clinic with locations in Toronto, New York, Chicago, Los Angeles, and Atlanta. Unlike Mindbloom, which went completely virtual in September of 2019, Field Trip offers an in-person ketamine experience at their spa-like facilities. Put The Wing, a Manhattan therapy office, and a yoga studio in a blender, and you'll get the vibe.
After a virtual visit with an M.D. to discuss your health history, you can sign up at Field Trip for "ketamine-assisted psychotherapy." A $2,500 treatment package at Field Trip includes 6 ketamine "exploratory sessions" (an in-office IV drip dose of ketamine with a licensed medical provider by your side), plus 3 "integration" sessions with a licensed therapist with psychedelic medicine training to process your experiences. (Field Trip's licensed therapists use research-backed psychotherapy techniques, the company says.)
"With ketamine in particular, it's a dissociative anaesthetic," says Ben Medrano, M.D., an integrative psychiatrist and Field Trip's medical director. "It allows you to dissociate enough from this level of identification with the painful emotions, so you can begin to look at that pain from different angles with the structure of the therapy."
It's not a totally out-there idea: Decades of research have shown that talk therapy (and talk therapy in combination with medication) is effective for mental health issues like depression and anxiety, as well as helping someone cope through other tough stuff like grief or a global pandemic. Research has shown that ketamine can help reduce even severe depressive symptoms within 24 hours. In 2019 a new version of ketamine ("esketamine") was FDA-approved specifically for treatment-resistant depression, though most clinics still use the original version of ketamine.
Some experts still see plenty of reasons for caution—at least for the time-being—and say it might not be the right treatment for everyone. "It seems to induce a one to 2 week alleviation of depression," said Charles S. Grob, M.D., Professor of Psychiatry and Pediatrics at UCLA School of Medicine, who has studied therapeutic uses of psychedelics. "The issue is, the depression returns."
As for the value of ketamine-assisted therapy, Dr. Grob said, "I have not seen much in the way of research that it works, or that it works more effectively than just ketamine alone."
There are also real risks to using ketamine. It is not recommended for people who have schizophrenia or certain heart issues, among other things. (FieldTrip and Mindbloom point out these issues are why they have screening performed by licensed providers in place.) But on top of that, there is a risk of becoming dependent on the drug. While it's not physically addictive in the same way opioids are, some people can develop a psychological dependency, Dr. Grob says.
Those currently making use of these services say they've had positive experiences.
Peter, a 40-something healthcare professional who asked that Insider conceal his identity, has been struggling with severe depression for the past two years. "In my lowest lows, literally, I was in the fetal position unable to get up off the floor for days," Peter says.
He started working with a traditional therapist three times a week, but did not want to try antidepressants."I don't think traditional medications allow you to work through your pain. They just allow you to function," he says. When he found out about Field Trip, he was immediately drawn to it because he'd read about ketamine's unique method of action in the brain, and he felt it could offer something other treatments couldn't. He wanted a chance to experience it legally, and with professional supervision.
After two sessions, he's already reporting profound benefits. "The experience of ketamine is far beyond what words can capture," he says. "For me, it helped me see a bigger picture, and that I don't have to ruminate. I can let go."
Watch: Psychologists debunk 25 mental-health myths
- Main content
Startups are betting on a psychedelic gold rush
A startup called Field Trip is opening clinics where they administer ketamine treatments. Other psychedelics, like MDMA and psilocybin, may follow.
by Rebecca Heilweil

For a long time, Chase Chewning had wanted to try a new type of psychotherapy that uses ketamine, a dissociative anesthetic that’s shown promise as a mental health treatment. Chewning, a veteran who has had several recreational experiences with MDMA and psilocybin, hoped the drug could help him with his PTSD, so he made an appointment at a Los Angeles ketamine therapy clinic operated by Field Trip Health. Having now completed two ketamine sessions , Chewning says his experience at Field Trip has indeed helped him make progress.
“In two sessions, I am profoundly closer to my work on my PTSD,” Chewning told Recode. “And [the treatment] left me with a lot of responsibility on some new work, but very, very exciting things, because I know I’m moving in the right direction, towards better mental health.”
Field Trip, a Canadian startup, is betting others could have similar experiences. In fact, the company is so confident in the promise of these drugs that it’s building 75 centers for psychedelic therapy over the next three years.
Although ketamine is legal if prescribed by a doctor, the Drug Enforcement Agency (DEA) lists psychedelics like psilocybin and MDMA in schedule 1 of the Controlled Substance Act, which says they have no medical value and a high potential for abuse . But there’s also growing evidence that psychedelics could lead to game-changing medications and, when combined with conventional therapy, may help people who aren’t seeing results through currently available treatments. Several US cities have already decriminalized psilocybin, the active ingredient in magic mushrooms, and the Food and Drug Administration (FDA) is overseeing clinical trials into using psychedelics to treat PTSD and depression.
This potentially revolutionary approach to mental health also represents a tremendous commercial opportunity for health care and pharmaceutical companies. But despite promising, privately funded studies into psychedelics, current government regulations prevent the wider availability of psychedelic therapy.
Field Trip currently offers ketamine treatments at six clinics in major US cities, including New York and Atlanta. The actual ketamine therapy session — Field Trip calls this a “psychedelic exploration session” — involves a patient receiving one or two shots of ketamine into their arm muscles, initiating a 45- to 90-minute hallucinogenic journey that’s supposed to help people disconnect from their normal selves. As the drug sets in, patients cover their eyes and listen to music as they’re coached by a therapist. The next day, patients return for a follow-up appointment called an “integration session” to reflect on the treatment.
“Whatever comes up in your session — new insights, perspectives — that can be fleeting if you don’t work to integrate that into your life,” Emily Hackenburg, Field Trip’s clinical director, told Recode. “Regardless of what psychedelic you’re using, preparation, journey, integration, that’s going to be the same.”
Field Trip says most patients undergo the ketamine program four to six times. The initial treatment, which includes a medical screening, an exploration session, and an integration session, costs $750. Because ketamine isn’t specifically approved for mental health applications by the FDA, the medication itself isn’t typically covered by insurance, though customers can try to get other aspects of the therapy reimbursed.
Though its treatments are expensive, Field Trip is growing quickly. In July, the company went public through a direct listing on Nasdaq and plans to offer ketamine treatments at 20 clinics in the US by early next year. Along the way, Field Trip is also setting itself up to be a huge player in an industry that largely doesn’t exist yet. While Field Trip’s US locations are currently limited to ketamine, the company hopes to offer more psychedelics, including MDMA, when the government approves their use. Field Trip is even developing its own psychedelic that’s meant to have similar effects as psilocybin, but with a much shorter trip.
The future of psychedelic therapy is also uncertain. While it seems likely that at least some psychedelic drugs will be approved for certain medical conditions in the years to come, it’s also possible that recreational use could be widely decriminalized or legalized. The status quo could also stay in place.
The US government has only recently begun to support and review research into psychedelics’ potential mental health benefits. But that slow approach means that just a few prominent companies and nonprofits are shaping much of the narrative surrounding the emerging psychedelics industry .
“This is really the most promising development in mental health care to come along, literally, in many decades. And that’s one reason why you don’t want a few companies controlling it,” says Mason Marks , a project lead at Harvard Law’s Petrie-Flom Center who focuses on psychedelics regulation.
Of course, not everyone is pleased that these startups could make psychedelics more mainstream. Some think these companies are capitalizing on a medical pathway for psychedelics that could ultimately exclude recreational users and make psychedelics more expensive and inaccessible. Others believe that psychedelics are being marketed as a cure-all that current research doesn’t support.
“Our experience with so-called pain clinics peddling untold amounts of opioids should be a cautionary tale,” Kevin Sabet, a former White House drug policy adviser who opposed legalizing cannabis , told Recode. “The psychedelics fad has reached a fever pitch far above and beyond what science tells us. We cannot forget the harmful potential and opportunity for manipulation by massive corporate interests.”
Nevertheless, it seems clear that the movement to make psychedelic therapy an accepted mental health treatment is gaining momentum.
A psychedelics renaissance could be coming
The origins of the government’s apprehensive approach to psychedelic-based mental health treatment stretch back decades. In the 1950s and ’60s, the federal government invested heavily into researching drugs like LSD and psilocybin. But after the Controlled Substances Act of 1972, federal funding into the possible benefits of psychedelics quickly evaporated.
That stance may be changing. In September, researchers at Johns Hopkins University received funding from the National Institute on Drug Abuse to investigate whether psilocybin could help people quit cigarettes. it appears to be the first federally funded direct study in decades of the mental health benefits of a traditional psychedelic drug. At the same time, the DEA, which keeps tight caps on how much psychedelics are available to US researchers, recently proposed increasing the nationwide availability of psilocybin from 30 grams to 1,500 grams.

There is also a growing number of efforts to make psychedelics more widely available not only to researchers but also to patients. In the last few years, Denver , Oakland , and Washington, DC , have decriminalized psilocybin, and in 2023, supervised psilocybin-based therapy will become legal in Oregon . Meanwhile, a psilocybin regimen for depression is in phase 2 trials , and an MDMA-assisted treatment for people with severe PTSD is currently in phase 3 clinical trials . The FDA has also already approved a Johnson & Johnson drug called Spravato, a nasal spray that’s derived from ketamine, to treat depression.
In anticipation of looser regulations, there’s a burgeoning psychedelic health care industry made up of companies that want to offer psychedelic treatments or develop new drugs based on psychedelic compounds. In addition to Field Trip, there are 31 publicly traded firms focused on psychedelics, and at least 18 more that are still private, according to the psychedelics industry tracker Psilocybin Alpha. Inspired by promising but limited research showing that psychedelics can help treat not only treatment-resistant depression but also addiction and end-of-life anxiety , venture capitalists, including Peter Thiel , have poured hundreds of millions of dollars into these companies.
“There’s a lot of enthusiasm. And that makes sense because there are many people who have suffered for many years for whom this has brought relief,” Sharmin Ghaznavi, an associate director of Massachusetts General Hospital’s Center for the Neuroscience of Psychedelics, told Recode. “But we have a lot that we need to learn, and we owe that to our patients.”
The government has been slow to support research into the potential benefits of psychedelics. That means philanthropies and private companies have funded almost all of the recent studies into the medical applications of drugs like MDMA and psilocybin. Many of those studies come with important caveats, including small sample sizes and unrepresentative patient pools. One 2018 analysis of 18 psychedelics studies found that 82 percent of the participants were white.
But even as research into psychedelics continues, companies are already developing everything from apps for guided trips and mushroom-facilitated retreats to psychedelic-assisted virtual reality experiences . After all, as with any big pharmaceutical breakthrough, the future of psychedelics could be extremely profitable.
How Field Trip plans to get ahead
Field Trip is well on its way to being a major player in the psychedelic health care industry. A centerpiece of Field Trip’s plan is the design of its clinics. The idea, the company says, is that psychedelics will need a brand new environment for medical care. Doctors’ offices are too sterile, and therapists’ offices don’t have the medical staff, time, or equipment to monitor patients. After all, trips on more intense psychedelic drugs require several hours and lots of supervision.
That’s why, at Field Trip’s New York location, there are serene rooms with reclining chairs and headphones for patients to use during their exploration sessions. Because ketamine can increase blood pressure, there are blood pressure monitors on-site, too. There are also rooms for post-trip reflection, where there are soft fur rugs, easels for drawing, and a gong. The space also includes a wall covered in live moss, a bubble-blowing machine, and several copies of Michael Pollan’s influential book about psychedelics, How to Change Your Mind .
“There’s lots of shoe companies out there, but Nike has a very prominent voice in that conversation,” Field Trip CEO Ronan Levy told Recode. “I want Field Trip to do that for psychedelics.”

While the company had about $100 million on hand at the end of June, Field Trip is currently making less than $1 million on patient services, according to its most recent quarterly report . One of the biggest challenges for Field Trip is that most people don’t have several thousand dollars lying around to spend on ketamine therapy. But if the FDA were to approve a psychedelic drug for a mental health condition, insurance companies may start to cover more Field Trip treatments, bringing them a huge new customer base.
There are certain conditions, like a history of psychosis or a ketamine allergy, that rule out Field Trip’s offering for some patients. Levy says the safety of ketamine has been well established and that Field Trip hasn’t had any medical issues. But others believe there is a litany of open questions.
Jeffrey Lieberman, a Columbia psychiatry professor, says the enthusiasm about psychedelics is outpacing the science, and he worries that mishaps could lead to backlash and a return to restrictions. If MDMA is approved for PTSD, for example, companies could end up prescribing the drug for other conditions that it hasn’t been approved for. That practice, which is sometimes called off-label prescribing, is already in place for ketamine. Lieberman added that we don’t fully understand the long-term safety of ketamine. There is also evidence ketamine clinics throughout the US are overhyping the drug’s abilities and not properly screening patients, acccording to a 2018 investigation by STAT.
There are other objections. A significant number of people oppose even the monitored use of psychedelics, including the 44 percent of Oregon residents who voted against the state’s recent measure to legalize a supervised psilocybin therapy model much like Field Trip’s. There are also psychedelic advocates who believe that allowing companies like Field Trip to do business will end up medicalizing and driving up the cost of psychedelics, which they think should be freely available .
The companies and people hoping to make psychedelic-based mental health care mainstream say this trend is about far more than just the drugs themselves.
“Taking a gram of mushrooms recreationally with your friends sitting around and giggling at YouTube music videos … it’s harmless,” Sanjay Singhal, a tech entrepreneur who directs the Nikean Foundation , a nonprofit that funds psychedelics research, told Recode. “But it’s completely different from taking five grams, knocking you out in the presence of a therapist for five hours while your brain processes whatever trauma, anxiety, emotional issues you might have.”
We’re bound to hear more about psychedelic therapy in the months to come. But even if psychedelics’ legal status remains the same, it’s clear to some patients that there’s a place for psychedelic therapy — even if it’s just the existing ketamine treatments — in our health care system. To Chewning, the veteran, these startups are addressing the demand for better mental health care and providing a new option for people who haven’t had success with traditional medications and therapy.
“I just look at what they’ve done for me personally, I look at what they have done for people I know,” he said. “We’re being put on a path toward a higher quality of life in the near future.”
- Future Perfect
- Health Care
- Mental Health
Most Popular
- Why I changed my mind about volunteering
- The massive Social Security number breach is actually a good thing
- The difference between American and UK Love Is Blind
- The staggering death toll of scientific lies
- Kamala Harris’s speech triggered a vintage Trump meltdown
Today, Explained
Understand the world with a daily explainer plus the most compelling stories of the day.
This is the title for the native ad
More in Technology

Freezing your credit files has never been easier. Here’s how to protect yourself.

Even OpenAI warns that chatting with an AI voice can breed “emotional reliance.”

However current companies do financially, the big AI safety challenges remain.

And a few things you can do about it.

The richest man in the world and the former president’s glitchy, cringeworthy interview, explained.

The FBI is now investigating the former president’s claim of Iranian interference with his campaign.
clock This article was published more than 1 year ago
I tried ketamine to treat my depression. It was terrifying.
The psychedelic therapy is said to help many people, but some like me have scary experiences.

My ears perked up in recent months when I began to hear the buzz about ketamine , the anesthetic and hallucinogenic drug that has found a new market as an antidepressant. Numerous credible studies have documented benefits, including that it is fast-acting, with patients sometimes showing improvement within a couple of days. And social and other media have featured doctors and patients describing it as “life changing,” with one user commenting that “I felt like a completely new person.”
For someone suffering from depression, that’s a tantalizing promise.
I’m 65 and for much of my life I’ve suffered from clinical depression, with two periods of suicidal ideation. Since 2002 I’ve taken a selective serotonin reuptake inhibitor, a type of antidepressant that has helped combat the day-to-day symptoms of this illness. Ditto the talk therapy I’ve participated in. But in the past year the medication’s impact seemed to be waning and my other efforts — exercise, meditation, socializing — didn’t seem to be helping as they once had. Having been down this road before, I recognized the dangers as the storm clouds gathered in my head.
As I read the buoyant reports of ketamine successes I decided it was time for me to try it — under the supervision of a professional therapist. With a referral from my therapist, soon enough I found myself on a new psychiatrist’s couch, a doctor specifically trained to administer the drug. The Food and Drug Administration approved the use of a nasal-spray form of ketamine for use in treatment-resistant, unipolar major depression. But the drug may be prescribed “off-label” for other depression and mental health conditions — though not for recreational use.
“At the dosage level administered to you, you are likely to experience mild anesthetic, anxiolytic [anti-anxiety], antidepressant and, potentially, psychedelic effects.” — Consent form
After determining that I was a medically healthy and otherwise eligible candidate, the psychiatrist — who trained at Yale’s School of Medicine, where much of the early ketamine research originated — briefed me in detail on all the possible side effects, short-term spikes in blood pressure, headache, nausea and vomiting. The nine-page consent form also included this sentence: “At the dosage level administered to you, you are likely to experience mild anesthetic, anxiolytic [anti-anxiety], antidepressant and, potentially, psychedelic effects.” The form also included commonly reported side effects such as “loss of sense of self, changes in the perception of time, dreamlike visions ... and feelings of connection, joy and peace.”
In looking back I realize I didn’t fully appreciate what all that meant. And so I went ahead and made an appointment for my first treatment session — together we would determine how many I’d need or want — remembering the importance of “set and setting,” which refers to a healthy mind-set and a relatively safe environment. (You would not want to take it, for example, if you were suicidal, or standing on a rooftop.)
Ketamine for depression: What it's like and who it can help
A first dose
Two weeks after the consultation I found myself in the doctor’s office, with late-afternoon sun shining through the office windows — and a blackout mask nearby. As soft music played in the background I took the first of two 100-milligram ketamine lozenges. I did what’s called the “swish and hold” for 10 minutes until it dissolved; then I swallowed.
Within 15 minutes, as I wrote in my journal the next day: “I experienced disequilibrium. Imbalance. Unable to find my place. Somewhere between scary and terrified.” Then came the blackness where I felt untethered, floating further and further away from any kind of anchor. I assumed I’d somehow put on the blackout mask — but I hadn’t.
According to the doctor’s notes (which he kept up with in real time during my journey), I told him, “Not sure I like this, feeling afraid of something I can’t see.”
I quickly became terrified of losing contact with him, talking incessantly to maintain the connection. When he switched from one chair to another, I panicked for a moment thinking he’d left me alone. (He had not.) He suggested I do what’s known as 4-7-8 breathing to curb my anxiety; it did. Completely engulfed by an unyielding darkness, I asked him, “Am I failing the experience?” And, “Where are the teal and fuchsia moments” that I had heard others speak of, or the peace and joy from the consent form? I kept talking: “Maybe I came in with unsaid expectations — that this would be a transformative experience. But wherever I go, there I am.”
His notes reveal we talked about “anticipatory grief,” as I began to weep about the prospect of my younger sister Julie possibly dying. (She has Stage 4 ovarian cancer.)
After about an hour I started to come down, regaining my equilibrium and opening my eyes to the darkness that had settled in around me and that I had glimpsed inside me.
Not long after the doctor asked me if I wanted to take a second lozenge, explaining that a second experience would likely be very different from the first. Exhausted and scared, I surprised myself when I said “yes.” I think I knew that if I didn’t try it again then, I never would.
Soon enough I was telling him, according to his notes, “Completely different with this lozenge — sad but not scared, feeling more tethered.” I talked more about losing Julie and the doctor suggested, “You will miss her wisdom and guidance.” Again I wept, asking, “Why do we have to feel?” because it was just too much. I thought back to the time when I had cancer myself, and how I’d been incapacitated by a different emotion: fear.
Once again I returned to the present, exhausted and somewhat nauseated. A friend came to drive me home, which is required because it takes several hours to fully recover. I’d made some mac ’n cheese ahead of time. I scarfed a bowl and fell asleep watching a silly Christmas movie.
The next morning I felt deflated. I’d expected a euphoric kind of experience based on what several friends had said. Trey Weaver, for example, told me he’d been treated almost a dozen times and his experience “feels like a reset from the physical tension and mental fatigue and hardship I endure from dealing with chronic pain.” That’s not at all what I experienced.
A few days later I had a follow-up appointment with the psychiatrist. Despite the mixed feelings I had about the lozenges, mainly the taste and upset stomach, I made another appointment three weeks hence, hopeful that the transformative experience would now be mine. The consent form had explained that “recent studies suggest the antidepressant response tends to be sustained with repeated use ...” And friends — and the doctor — had told me that it can take several sessions for ketamine to work, although many who suffer from depression realize almost immediate effects. This time the doctor would be injecting 50 milligrams of ketamine intramuscularly.
Three minutes later, more scared than excited, I told the doctor, “I have liftoff.”
In fact, I saw myself strapped to a rocket shooting up into space — again, a deep black space. I very quickly lost track of time, but I also lost almost all sensation in my mouth, a result of ketamine’s analgesic and anesthetic properties. I couldn’t feel my lips and began tapping on my face in search of them. No luck. Panic. Suddenly, my throat disappeared — no feeling when I swallowed. I could only “see” a black hole where it had been. I tried not to swallow, fearful that I’d choke to death on my own saliva. More panic.
According to the psychiatrist’s notes I asked out loud, “Am I okay?” (In my head I recall shouting something more like, “GET ME OUT OF HERE!”)
I soon felt completely immobilized, trapped in my body. I started to recall a magazine story I’d written a long time ago about a woman who lived in what’s known as a “locked-in” state. (According to the Cleveland Clinic, people with locked-in syndrome “have total paralysis but still have consciousness and their normal cognitive abilities.”) I saw myself in a glass coffin looking out into the dark universe, although I’d see flashes of deeply hued magenta and chartreuse from time to time.
According to reputable studies, ketamine can be life-changing for a significant majority — as much as three-quarters — of those who take it for depression. That leaves 25 percent, like me, who are not so fortunate.
The doctor’s notes say I reached out to him with my left hand, a manifestation of my distress. I felt him clasp it. “This is my lifeline,” I thought to myself, holding on to his hand for about 15 minutes as I tried to use Morse code to communicate “SOS.” (Alas, I don’t know Morse code so I’m not sure what I communicated.)
“Was I going to be locked in forever?” I thought to myself, floating through space, untethered to my family, friends and my cocker spaniel at home. The answer appeared to be yes, because with no real sense of time, I began to feel as though months were passing.
I wondered, “What had I done wrong to put myself in such danger?” I had taken all the proper steps before starting this journey, and still somehow I felt something awful had happened to me. I had a “sense of sliding into a death experience.” I was dying, although I wasn’t frightened by that. Eventually I gave in and slid through the tunnel toward the light, accepting my fate.
Forty-five minutes after the injection I started reentry, touching my mouth with my fingers, feeling my throat, hearing myself speak out loud (not necessarily coherently). The doctor reported in his notes that I told him, “Oh my gosh, I died.”
That evening I texted the psychiatrist: “I’m ok. But I feel like today’s journey was too much, too fast, too dark.” He replied quickly, saying he hoped “tomorrow finds your fears less prominent.”
The next handful of days did not prove easier. When I texted the psychiatrist he was responsive and kind, and suggested the timing of our sessions might not have been best, given my worries about my sister.
“Psychedelic experiences can be hard, regardless of set and setting. Integration is important, and so is giving it time to settle,” he texted back.
The aftereffects
In the days that followed I still didn’t feel like myself. Detached. Untethered. Scared. In a world of my own. Several friends noticed this difference in me, with one asking me directly if I was at risk of self-harm.
During my next appointment the doctor suggested I increase my daily dose of the antidepressant I take. I could not do it quickly enough. Within several days I began to settle, feel better, more like “me.”
And just the thought of trying ketamine again made me feel anxious.
Where does that leave me? According to reputable studies, ketamine can be life-changing for a significant majority — as much as three-quarters — of those who take it for depression. That leaves 25 percent, like me, who are not so fortunate.
I asked John Krystal, chief of psychiatry and behavioral health at Yale-New Haven Hospital and a leading authority on ketamine use for depression, about my experience. “There is a risk that some patients will have extremely upsetting experiences during treatment [with] ketamine or psychedelics,” he said. “The experience of losing control of the form and content of their thought processes and the altered sensory experiences are, themselves, potentially traumatic experiences.”
I wish I’d understood that better beforehand so that my expectations would have been better aligned with my experience. Still, Krystal continued, “When patients are well prepared for the experiences, supported as they occur, and debriefed afterwards, the risk of lasting negative effects is substantially reduced and the potential for personal growth is enhanced.”
I was glad to hear that the negative feelings would probably dissipate — and they did over a period of six weeks — and I might even discover some delayed benefits to the treatment (still waiting). Perhaps this wasn’t the right time for me to try ketamine. But this was when I felt that I needed it most. And I — like so many others who suffer from debilitating depression — had been willing to grab for a much-talked about lifeline to help me through the storm. It was not, however, a lifesaver for me.
Sign up for the Well+Being newsletter, your source of expert advice and simple tips to help you live well every day
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
This weightlifting workout in your 60s can preserve strength for years
Are white noise machines bad ? Here’s what the latest science says.
I prepared for my knee replacement surgery . But I had a lot to learn.
Electric toothbrushes are better. But the right technique matters more.
Avocado hand : How to avoid an injury so common that surgeons have a name for it
Making new friends can be hard. Here are 5 ways to make 1 friend a year .

Advertisement
Supported by
‘Shoot Me Up With a Big One’: The Pain of Matthew Perry’s Last Days
Court papers show that Mr. Perry, the “Friends” star who had long struggled with addiction, was increasingly taking ketamine, a powerful anesthetic, in the days before he died.
- Share full article

By Julia Jacobs and Matt Stevens
On the day Matthew Perry died , his live-in personal assistant gave him his first ketamine shot of the morning at around 8:30 a.m. About four hours later, while Mr. Perry watched a movie at his home in Los Angeles, the assistant gave him another injection.
It was only about 40 minutes later that Mr. Perry wanted another shot, the assistant, Kenneth Iwamasa, recalled in a plea agreement that he signed.
“Shoot me up with a big one,” Mr. Perry told Mr. Iwamasa, according to the agreement, and asked him to prepare his hot tub.
So Mr. Iwamasa filled a syringe with ketamine, gave his boss a third shot and left the house to run some errands, according to court papers. When he returned, he found Mr. Perry face down in the water, dead.
Mr. Iwamasa was one of five people who the authorities in California said this week had been charged with a conspiracy to distribute ketamine , a powerful anesthetic, to Mr. Perry. The defendants also included two doctors, a woman accused of being a dealer and an acquaintance who pleaded guilty to acting as a middleman.
Mr. Perry, a beloved figure who rose to fame playing Chandler Bing on the sitcom “Friends,” had long struggled with addiction. Court papers filed in the case shed light on the desperate weeks leading up to Mr. Perry’s death on Oct. 28 at the age of 54.
In his last days, law enforcement officials said, he appeared to become increasingly reliant on ketamine, and eager to find illegal sources of it after doctors at a local clinic had refused to increase his dosage.
There were warning signs that it was dangerous. The court papers refer to several instances in which Mr. Perry experienced adverse effects from the drug, including when his assistant found him unconscious at his home and observed him losing the ability to speak or move after a large dose.
In the indictment, which followed a seven-month investigation and grand jury proceedings, prosecutors accused several of the defendants of enabling Mr. Perry’s ketamine use despite being aware of his history of drug abuse and addiction, and his attempts to stay sober.
This account of Mr. Perry’s last days was drawn from the indictment and from the plea agreements reached by Mr. Iwamasa and two of the other defendants. Efforts to reach the defendants were unsuccessful; on Thursday, Dr. Salvador Plasencia and Jasveen Sangha, whose trials are scheduled for October, pleaded not guilty.
“These defendants took advantage of Mr. Perry’s addiction issues to enrich themselves,” Martin Estrada, the United States attorney for the Central District of California, said at a news conference Thursday in downtown Los Angeles.
“They knew what they were doing was wrong,” he continued. “They knew what they were doing was risking great danger to Mr. Perry. But they did it anyway. In the end, these defendants were more interested in profiting off Mr. Perry than caring for his well-being.”
‘I Just Ran Out’
As Mr. Perry’s personal assistant, Mr. Iwamasa was tasked with coordinating his doctor’s appointments and making sure he took the proper medication.
Ketamine, a strong anesthetic with psychedelic properties , is sometimes used as an alternative therapy for depression, anxiety and other mental health problems. It is also used recreationally.
Mr. Perry had earlier pursued ketamine therapy, law enforcement officials said. But when doctors at a local clinic refused to increase his dosage, they said, he sought the drug elsewhere. In September, Mr. Perry asked Mr. Iwamasa to procure him ketamine illegally, according to the plea agreement.
Mr. Iwamasa was introduced to Dr. Salvador Plasencia, a physician who was later charged in the case, as he sought the drugs.
At one point Dr. Plasencia mused on the money he stood to make with a friend, Dr. Mark Chavez. “I wonder how much this moron will pay,” Dr. Plasencia texted Dr. Chavez, who prosecutors said later supplied him with a total of 22 vials of ketamine and ketamine lozenges obtained through a fraudulent prescription for the drug. “Lets find out.” Dr. Chavez agreed to plead guilty to one count of conspiracy to distribute ketamine.
Dr. Plasencia, known as “Dr. P.,” soon instructed Mr. Iwamasa on how and where to inject ketamine into Mr. Perry’s body.
“Found the sweet spot but trying different places led to running out,” Mr. Iwamasa texted Dr. Plasencia on Oct. 4, according to court documents.
Over the next several days, Mr. Iwamasa’s requests for ketamine became more urgent.
“I just ran out,” Mr. Iwamasa texted the doctor, who replied he had two vials to sell him if the assistant could meet him in downtown Santa Monica.
That week, Dr. Plasencia met Mr. Perry and his assistant in a parking lot near an aquarium in Long Beach, Calif. He injected the actor in the back seat of the car, passing along multiple additional vials. Mr. Perry would ultimately pay at least $55,000 to Dr. Plasencia for ketamine over a period of about a month, according to court papers.
Searching for a New Supply
The actor and his assistant were beginning to look for additional sources to keep up their supply of the drug.
Mr. Perry began communicating with a man named Erik Fleming, with whom he shared a mutual friend. Mr. Fleming, who later agreed to cooperate with law enforcement, texted Mr. Perry on Oct. 10 that he could sell him ketamine at a “good price,” as long as he received a tip for brokering the deal.
Mr. Fleming was put in touch with Mr. Iwamasa to work out the details, texting him an image of a ketamine vial with a photograph of a horse on the packaging. (The drug is commonly used as a veterinary tranquilizer.)
The next day, Mr. Fleming showed Mr. Iwamasa screenshots of his communications with his source, a woman named Jasveen Sangha, whom Mr. Fleming described as working with “high end” clients and celebrities. “If it were not great stuff she’d lose her business,” Mr. Fleming wrote of Ms. Sangha’s supply.
Mr. Iwamasa texted Mr. Fleming that his boss was “only interested in the unmarked ones not the horsey version,” according to court papers.
“I did some calling around about the Mexican stuff and it’s fine for people too,” Mr. Fleming later responded.
On the same day that Mr. Perry received a legal ketamine infusion treatment from another doctor at a medical office, Dr. Plasencia visited Mr. Perry’s home and administered him a “large dose” of ketamine, according to Mr. Iwamasa’s account to law enforcement. Mr. Perry froze up, was unable to speak or move, and experienced a spike in blood pressure; Mr. Iwamasa and the doctor struggled to move him onto a couch.
Dr. Plasencia “stated something to the effect of, ‘let’s not do that again,’” the court papers said. But he continued to offer more ketamine, the papers said.
The next day, Mr. Fleming delivered a sample vial of ketamine to Mr. Perry’s home for $180. Satisfied with the drug, Mr. Iwamasa asked for more. Mr. Fleming delivered 25 vials for $6,000, including $500 for his own work, on Oct. 14.
Ten days later, Mr. Fleming delivered another 25 vials, along with ketamine lollipops that Ms. Sangha included as a bonus.
Mr. Iwamasa and Mr. Fleming both agreed to sign plea agreements, giving officials a window into Mr. Perry’s final days. Dr. Chavez eventually began cooperating with law enforcement as well. Mr. Iwamasa faces up to 15 years in prison, Mr. Fleming up to 25 years and Dr. Chavez up to a decade.
A Half-Dozen Shots per Day
In the final days leading up to the actor’s death, Mr. Iwamasa injected Mr. Perry six to eight times per day. At least twice, he found Mr. Perry unconscious at his home, the assistant told law enforcement.
On Oct. 28, after giving Mr. Perry three shots and later finding him dead, Mr. Iwamasa cleaned up the bottles and syringes left in the house, according to Mr. Fleming’s account of a conversation they later had. Mr. Iwamasa later told law enforcement officials that all of the injections administered that day had come from the supply delivered by Mr. Fleming.
That day Ms. Sangha deleted her text messages with Mr. Fleming from the app Signal and instructed him to “delete all our messages,” according to law enforcement officials.
In a text message, Mr. Fleming assured Ms. Sangha, who prosecutors said was known as “the Ketamine Queen,” that he was “90% sure everyone is protected,” saying he had dealt only with Mr. Perry’s assistant, not Mr. Perry.
“Does K stay in your system or is it immediately flushed out,” Mr. Fleming asked her.
In December the Los Angeles County medical examiner’s office said that Mr. Perry had died of the “acute effects” of ketamine . The autopsy report noted that the level of ketamine found in his blood was equivalent to the amount used for general anesthesia.
Jill Cowan contributed reporting from Los Angeles. Kirsten Noyes contributed research.
Julia Jacobs is an arts and culture reporter who often covers legal issues for The Times. More about Julia Jacobs
Matt Stevens writes about arts and culture news for The Times. More about Matt Stevens
The depths of Matthew Perry's addiction: 6 to 8 shots a day and $55K for a month of ketamine
LOS ANGELES — “Friends” actor Matthew Perry was experiencing an out-of-control ketamine addiction, injecting the drug six to eight times a day, before his accidental overdose death , prosecutors say.
Five people have been charged in connection with Perry’s death, including his personal assistant, Kenneth Iwamasa, and one of those accused of providing the drug, Dr. Salvador Plasencia.
In court documents filed Thursday, federal prosecutors accuse Plasencia of telling a patient that Perry was “too far gone and spiraling in his addiction” the week before he died but that he still offered to sell Perry ketamine through Iwamasa anyway.
Perry had been undergoing ketamine infusion therapy to treat depression and anxiety , but it was not the supervised therapy doses that killed him. His last session was more than a week before his death.

According to prosecutors, Perry had been seeking out unsupervised doses of the controlled substance and had developed an “out of control” dependence on it. Ketamine, an anesthetic with psychedelic properties, is a popular party drug that has recently been found to be a promising alternative treatment for some mental illnesses but carries serious medical risks.
Perry, 54, was found face down in the heated end of a pool at his Pacific Palisades home on Oct. 28. When he died, the levels of ketamine in his body were high — equivalent to the amount used for general anesthesia during surgery, according to the Los Angeles County Medical Examiner’s Office.
His assistant, Iwamasa, 59, pleaded guilty on Aug. 7 to one count of conspiracy to distribute ketamine causing a death and admitted having repeatedly injected Perry without medical training, according to prosecutors.
The court documents laying out Iwamasa’s plea agreement detail the depths of Perry’s addiction.
Iwamasa was accused of injecting Perry the day he died at 8:30 a.m. and again at 12:45 p.m. while Perry was watching a movie, the agreement said.
“Approximately 40 minutes later, Victim M.P. asked defendant to prepare the jacuzzi for Victim M.P. and told defendant, ‘shoot me up with a big one,’ referring to another shot of ketamine,” the document said.
After he injected Perry with the third shot in six hours, Iwamasa went to run errands, the documents say. He found Perry face down in the pool when he returned to the home, according to the plea agreement.
Iwamasa told authorities he began injecting Perry roughly a month before he died, after Perry was introduced to Plasencia around Sept. 30. He alleged that Plasencia sold Perry liquid ketamine, as well as ketamine lozenges, according to court documents.
Plasencia, 42, was arrested Thursday in Southern California and charged with one count of conspiracy to distribute ketamine. He pleaded not guilty in court Thursday afternoon. His lawyer did not respond to a request for comment.
Federal prosecutors said Plasencia taught Iwamasa how to administer the drug through intramuscular injection, even though Iwamasa had no medical experience or education.
Perry then instructed Iwamasa to stay in touch with Plasencia to buy more vials. The plea agreement recounts almost daily communications between Plasencia and Iwamasa to arrange more purchases in the next two weeks.
On Oct. 12, about two weeks before he died, Perry had a ketamine infusion with a doctor, but Plasencia was still contacted after the treatment for more, according to prosecutors. According to the plea agreement document, Plasencia agreed to meet at Perry’s home later that day and administered a “large dose of ketamine.”
Perry had a bad reaction to that dose, it said. His blood pressure spiked, his body began to “freeze up,” and he could not talk or move, prosecutors said. Plasencia left additional vials of ketamine for Perry at the house, despite Perry’s adverse reaction to it, prosecutors alleged.
According to prosecutors, the next day Perry instructed Iwamasa to obtain more ketamine from a different supplier, an acquaintance Iwamasa had previously gotten into contact with named Erik Fleming.
Fleming, 54, pleaded guilty on Aug. 8 to one count of conspiracy to distribute ketamine and one count of distribution of ketamine resulting in death.
Perry paid Plasencia — through his assistant — at least $55,000 for ketamine in the month before he died, Iwamasa’s plea agreement says. Fleming was paid about $12,000 for two deals, one of them just days before Perry died.
Another doctor was arrested Thursday and charged, and a third person has agreed to plead guilty in connection with Perry’s death.
Perry, who rose to fame on the beloved sitcom series “Friends,” was vocal about his addiction issues. He said in a 2022 interview on the “ Q with Tom Power ” podcast that he could not watch “Friends” because he could tell by his weight what substance he was abusing: alcohol, opiates or cocaine.
Perry wrote in his memoir that he “should be dead” after years of addiction and that his sobriety gave him purpose.
In 2013, Perry was given the Champion of Recovery award from the White House Office of National Drug Control Policy. The same year, he converted his Malibu residence into a sober-living home that operated for two years.
“I’ve said this for a long time: When I die, I don’t want ‘Friends’ to be the first thing that’s mentioned,” Perry said the year before he died . “I want [helping people] to be the first thing that’s mentioned. And I’m going to live the rest of my life proving that.”
Andrew Blankstein is an investigative reporter for NBC News. He covers the Western U.S., specializing in crime, courts and homeland security.
Doha Madani is a senior breaking news reporter for NBC News. Pronouns: she/her.
Matthew Perry’s doctor still seeing patients after being charged in actor’s ketamine death
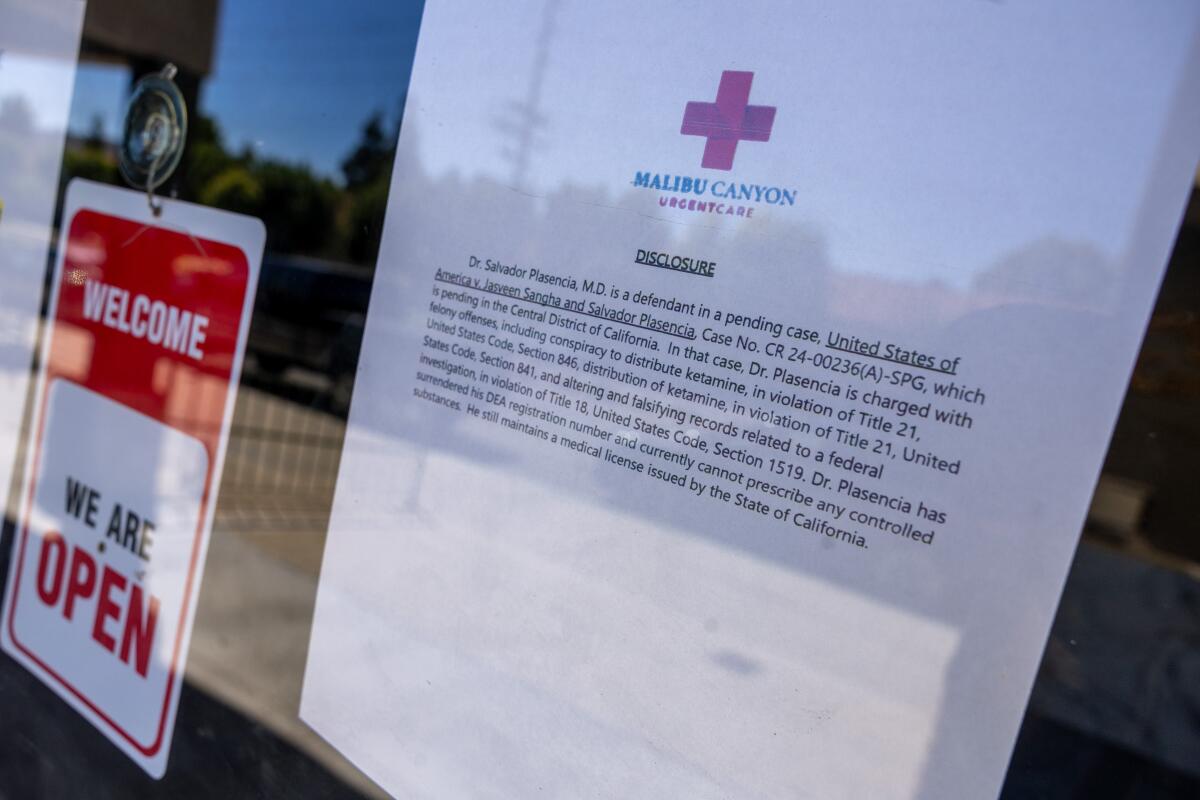
- Copy Link URL Copied!
A physician charged with conspiring to distribute ketamine in the wake of Matthew Perry’s death is still seeing patients at the urgent care facility he operates in Calabasas.
Now facing felony charges, Dr. Salvador Plasencia is forbidden by the Drug Enforcement Administration from prescribing controlled substances, but he can, under certain conditions, continue to practice medicine, according to federal officials.
He has surrendered his DEA registration number, according to a sign posted Wednesday on the door of Malibu Canyon Urgent Care. The sign noted that he “still maintains a medical license issued by the State of California.”
Ciaran McEvoy, a spokesman for U.S. Atty. Martin Estrada’s office in Los Angeles, said Plasencia and another doctor charged in Perry’s death — Mark Chavez — have both surrendered their DEA licenses and therefore “cannot prescribe controlled substances.”
According to the state medical board, Plasencia’s medical license is active through October.

Matthew Perry’s shocking last month on ketamine: ‘I wonder how much this moron will pay’
In announcing arrests in the death of “Friends” star Matthew Perry, authorities unveiled a disturbing narrative of the weeks leading up to his final day.
Aug. 16, 2024
The 42-year-old physician, known as Dr. P., was charged last week in the October death of the “Friends” star, along with Chavez, Perry’s live-in personal assistant and two alleged drug dealers.
Plasencia is facing one count of conspiracy to distribute ketamine, seven counts of distribution of ketamine and two counts of altering and falsifying documents or records related to the federal investigation. If convicted, he faces 10 years for each ketamine-related charge and 20 years for each falsification charge.
Despite the charges, Plasencia is allowed to continue practicing medicine, his attorney, Stefan Sacks, told The Times.

“The conditions are that he disclose in writing the existence of the pending federal case, and the fact that he cannot prescribe controlled substances. Patients are then required to sign a written consent form for treatment,” Sacks said. “So basically the requirement is disclosure and informed consent.”
On Wednesday, a woman approached the Calabasas clinic, read the notice on the door regarding the charges against Plasencia and then quickly returned to her vehicle.
Sacks said he would not comment further on the charges against Plasencia until he receives discovery from the U.S. attorney’s office detailing the allegations against his client. The physician has pleaded not guilty to all charges and was released in lieu of $100,000 bail. He is due back in court in October.

A dealer known as ‘Ketamine Queen’ and 2 doctors among 5 charged in death of Matthew Perry
Federal authorities have filed drug charges against five individuals, including two doctors, in connection with the death of ‘Friends’ star Matthew Perry.
Aug. 15, 2024
Perry, 54, was found dead in the hot tub of his Pacific Palisades home on Oct. 28. He died from “acute effects of ketamine,” according to the Los Angeles County Medical Examiner’s Office.
Plasencia is accused of acquiring the ketamine for Perry and acting outside the scope of professional practice. Authorities say he not only distributed the drug that killed the actor, he also taught Perry’s personal assistant, Kenneth Iwamasa, how to inject it into the actor. Iwamasa is accused of giving Perry the fatal dose.
Perry, who had long been open about his challenges with drug and alcohol addiction , had sought treatment for depression and anxiety before his death, going to a local clinic where he became addicted to intravenous ketamine, DEA Administrator Anne Milgram said. When clinic doctors refused to increase his dosage, he turned to outside sources, Milgram said.
In late September, about a month before Perry’s death, Plasencia learned the actor was interested in obtaining ketamine, a legal medication commonly used as an anesthetic, according to charging documents in the case. The drug can be abused recreationally, with users drawn to it for its dissociative effects.
After learning of Perry’s interest, Plasencia contacted Chavez, who previously operated a ketamine clinic, to obtain the drug to sell to the actor, authorities said. In text messages to Chavez, Plasencia discussed how much to charge Perry for the ketamine, stating, “I wonder how much this moron will pay” and “Lets find out,” according to court records.

The ketamine boom: How the wealthy are getting their hands on the in-demand drug
Medical and law enforcement officials say the wealthy are financing the ketamine black market while more prescriptions and specialized clinics are emerging.
May 30, 2024
In the weeks that followed, the doctors distributed 20 vials of ketamine to Perry for $55,000 in cash, charging him $2,000 for a vial that cost Chavez $12, according to federal prosecutors and court records.
Court records show that by mid-October, Iwamasa also began obtaining ketamine for Perry from Jasveen Sangha, known as the “Ketamine Queen,” and Hollywood producer Erik Fleming, who provided the drug at a lower cost than the doctors were charging. Sangha sold about 50 vials of the drug to the actor, with Fleming delivering the product, for $11,000, authorities said.
Like Plasencia, Sangha, 41, is facing charges that include conspiracy to distribute ketamine, distribution of the drug resulting in death, possession with intent to distribute and altering and falsifying records related to a federal investigation, according to the indictment.
Fleming, 54, pleaded guilty this month to one count of conspiracy to distribute ketamine and one count of distribution of ketamine resulting in death.
Iwamasa, 59, pleaded guilty to a count of conspiracy to distribute ketamine causing death. He also admitted injecting Perry with ketamine without medical training, including performing several injections on the actor the day he died, authorities said.
More to Read

Fake doctor injured a patient while pretending to be a cosmetic surgeon, L.A. prosecutors say
Aug. 25, 2024

Editorial: Let’s not learn the wrong lessons from Matthew Perry’s ketamine tragedy
Aug. 23, 2024

L.A.’s ‘Ketamine Queen’ lived a celebrity-studded life. Now she’s been charged in Matthew Perry’s death
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.

Richard Winton is an investigative crime writer for the Los Angeles Times and part of the team that won the Pulitzer Prize for public service in 2011. Known as @lacrimes on Twitter, during almost 30 years at The Times he also has been part of the breaking news staff that won Pulitzers in 1998, 2004 and 2016.
More From the Los Angeles Times

Charli XCX ‘happy to help’ after Kamala Harris tweet influences presidential push

Mira Mesa resident accused of crafting makeshift bombs to try to rob ATMs
Does it matter if Babe Ruth ‘called shot’ in 1932 World Series? His jersey sells for $24 million

An Albertsons and Kroger merger would remake grocery shopping. A judge must decide whether to halt it.

IMAGES
COMMENTS
The infusions are accompanied by psychedelic "trips.". That's just part of ketamine. In the beginning, I believed that the trip didn't matter — the drug got in me regardless of if the trip was "good" or "bad.". A lot of my trips are "bad.". I believe this is largely because of complex post-traumatic stress disorder ( C-PTSD ).
Ketamine trips are uncannily like near-death experiences. is the editor of Psyche. A cognitive neuroscientist by training, his books include The Rough Guide to Psychology (2011), Great Myths of the Brain (2014) and Be Who You Want: Unlocking the Science of Personality Change (2021). Published in association with The British Psychological ...
Like other hallucinogens, ketamine can be used recreationally to achieve a hallucinogenic experience known as K-hole. About 0.13% of American adults used ketamine in the past year,. This type of ...
A Stanford anesthesiologist deconstructs the component parts of what it means to undergo a psychedelic trip. ... in a person's belief that taking psilocybin or ketamine is going to give them a ...
It's also possible that an individual having a ketamine treatment may experience a "bad trip," colloquially known as "falling into a k-hole." A k-hole is an acute, dissociative state that results ...
Ketamine causes what doctors call a "dissociative experience" and what most anyone else would call a "trip." That's how it became a club drug, called K, Special K, Super K, and Vitamin K ...
Ketamine, approved as an anesthetic in 1970, is emerging as a major alternative mental health treatment. ... It has the potential to send users down a "K-hole," otherwise known as a bad trip, and ...
Many people compare taking ketamine for depression to taking a psychedelic "trip." While the experience is different for everyone, many people feel a sense of overwhelming calm and relaxation .
Federal authorities said their investigation into Perry's death uncovered a "broad underground criminal network" of drug suppliers who distributed large quantities of ketamine across Los Angeles.
As access grows, we need better research and education on bad trips. by Oshan Jarow. Nov 10, 2023, 12:30 PM UTC. wildpixel/Getty Images.
Ketamine is a dissociative anesthetic that has some hallucinogenic effects. It distorts perceptions of sight and sound and makes the user feel disconnected and not in control. It is an injectable, short-acting anesthetic for use in humans and animals. It is referred to as a "dissociative anesthetic" because it makes patients feel detached ...
Last month, Field Trip, a chain of ketamine clinics, was listed on the Nasdaq. Plus, ketamine clinics have been popping up like Starbucks in major urban areas.
Ketamine Wellness Centers, a brick-and-mortar chain, shut down in March 2023 due to funding issues. Patients, some of them suicidally depressed, lost access to treatment immediately.
Inside, according to Dr David Belin, a behavioural science lecturer at the University of Cambridge, "you're disrupting the activating system of the brain - the glutamate system - which ...
At Field Trip Health, one IM injection costs $750, and Mindbloom charges $89 a week for three months ($1,060) for new patients, which includes six ketamine treatments. Returning clients pay $59 ...
At the start of my second session, I blurted out a silly thought: "An infusion of ketamine is like taking a two-hour Uber trip with a clown." (Luckily for me, the anesthesiologist didn't ...
According to Shah, feeling the effects of ketamine within 24 hours of treatment is typical. "It is the most rapid-acting treatment for depression," he said. After the final infusion, I had the ...
Patients receiving ketamine-assisted psychotherapy often sit in a controlled environment, such as this one seen at Field Trip psychedelic therapy clinic in Toronto, Ontario, Canada.
Two main types of ketamine are used to treat major depression that hasn't responded to two or more medications (treatment-resistant depression). Racemic ketamine, which is most often given as an infusion into the bloodstream. This is sometimes called intravenous, or IV, ketamine. It is a mixture of two mirror-image molecules: "R" and "S" ketamine.
My first ketamine trip was a totally out-of-body, dissociative experience. I didn't see the Kool-Aid colors you always associate with psychedelics, but there were pleasant, low-level visuals.
At Field Trip, a national chain of clinics that has offered ketamine-assisted psychotherapy for several mental health conditions since 2019, patients first undergo a screening to see if they ...
Like most ketamine clinics, Field Trip encourages an initial set of four to six infusions spaced out across two to four weeks, with boosters available on an as-needed basis thereafter. The first ...
The death of Mr. Perry, a beloved figure who starred on the sitcom "Friends," placed a harsh spotlight on the illegal ketamine trade. Five people, including two doctors, were arrested and ...
A $2,500 treatment package at Field Trip includes 6 ketamine "exploratory sessions" (an in-office IV drip dose of ketamine with a licensed medical provider by your side), plus 3 "integration ...
Field Trip says most patients undergo the ketamine program four to six times. The initial treatment, which includes a medical screening, an exploration session, and an integration session, costs $750.
This article was published more than 1 year ago. I tried ketamine to treat my depression. It was terrifying. The psychedelic therapy is said to help many people, but some like me have scary ...
Ketamine is an anaesthetic that can be used to treat depression, anxiety and pain in a medical setting. However, it also has dissociative effects - meaning it can distort perceptions of sight ...
On the day Matthew Perry died, his live-in personal assistant gave him his first ketamine shot of the morning at around 8:30 a.m.About four hours later, while Mr. Perry watched a movie at his home ...
Ketamine, an anesthetic with psychedelic properties, is a popular party drug that has recently been found to be a promising alternative treatment for some mental illnesses but carries serious ...
In the weeks that followed, the doctors distributed 20 vials of ketamine to Perry for $55,000 in cash, charging him $2,000 for a vial that cost Chavez $12, according to federal prosecutors and ...